Beruflich Dokumente
Kultur Dokumente
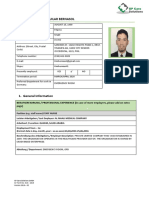
Soft Tissue Pathology PPDS BEDAH 06 - Kecil
Hochgeladen von
shevinesaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Soft Tissue Pathology PPDS BEDAH 06 - Kecil
Hochgeladen von
shevinesaCopyright:
Verfügbare Formate
Soft Tissue Pathology
KULIAH PPDS
BEDAH-2006
Nurjati Siregar
OBJECTIVES
To know classification of soft tissue tumor
To know the biological behaviour of soft tissue
tumor (benign vs malignant)
To know characteristic features of benign and
malignant soft tissue tumors (size, location, age,
gender)
To know the limitation of biopsy (FNA, core,
incision) in diagnosis
To know how to fill pathology request form
Soft Tissue
Fibrous tissue
Adipose tissue
Synovial tissue
Skeletal muscle
Blood vessels
Peripheral nerves
Soft tissue tumor
Majority are benign
High cure rate after surgical excision
Malignant < 1%
> 50 STS histological types
Unique clinical, prognostic and therapeutic
features
Close interaction pathologist-surgeon-
radiologist-oncologist --- 5 y survival rate: 65-
75% of STS in limbs
EPIDEMIOLOGY
Benign > 100 X malignant/sarcoma
Benign: 3000 in 1.000.000
Malignant: 30 in 1.000.000
Benign STT
33% lipomas,
33% fibrohistiocytic tumor
10% vascular tumor
5% nerve sheet
Relation between type of tumor-symptom-
location-age-gender.
Lipoma: painless, rare in hand, very
uncommon in children
Soft tissue sarcomas (STS) (1)
Occurs anywhere:
75% in extremities (most common in thigh)
10% in trunk wall and retroperitoneum
Male predominance (slightly)
More common in elderly (median age 65
y)
In extremity and trunk-wall:
1/3 superficial, diameter 5 cm
2/3 deep seated with diameter 9 cm
Retroperitoneal:
Much larger
10% have detectable metastasis (lung)
33% because of metast in lung
Soft tissue sarcomas (STS)
(2)
75% classified as MFH-like sarcoma,
liposarcoma, leiomyosarcoma, synovial
sarcoma and MPNST
75% of those are in grade 2 and 3
Children: embryonal rhabdomyosarcoma
Young adult: synovial sarcoma
Elderly: pleomorphic HG sarcoma,
liposarcoma and leiomyosarcoma
Soft tissue sarcomas (STS)(3)
ETIOLOGY
Unknown
Genetic
Environmental factors
Irradiation
Viral infections
Immune deficiency
Chemical carcinogenesis: phenoxyacetic
herbicides, chlorophenols, dioxin
Tumors and Tumor-Like
Conditions of Fibrous Tissue
Benign
Nodular Fasciitis
Palmar fibromatosis
Abdominal fibromatosis (desmoid tumor)
Malignant
Fibrosarcoma
Tumor differentiation
Score 1.
Sarcoma closely resembling normal adult
mesenchymal tissue (e.g. low grade
leiomyosarcoma)
Score 2.
Sarcoma for which histological typing is
certain (e.g. myxoid liposarcoma)
Score 3.
Embryonal and undifferentiated sarcomas of
doubtful type, synovial sarcoma,
osteosarcomas, PNET
Mitotic count
Score 1: 0-9 mitoses/10 HPF
Score 2: 10-19 mitoses/ 10 HPF
Score 3: 20 mitoses/ 10HPF.
Tumor necrosis
Score 0: no necrosis
Score 1: < 50% tumor necrosis
Score 2: 50% tumor necrosis
Histological grade
Grade 1: total score 2,3
Grade 2: total score 4,5
Grade 3: total score 6,7,8
FNLCC (French Federation
Nationale des Centres
de Lutte Contre le Cancer
NCI (United States National
Cancer Institute)
Grading
Should be used only for untreated primary STS
Should be performed on representative and well
processed material.
Not a substitute for a histologic diagnosis and
does not differentiate benign and malignant
lesion
Not applicable to all STS
(e.g MPNST, angiosarcoma, extraskeletal
myxoid chondrosarcoma, alveolar soft part
sarcoma, clear cell sarcoma and epithelioid
sarcoma)
Staging
Based on both histological and clinical
information (UICC) and AJCC
Appears to be clinically useful and of
prognostic value
TNM incorporates histological grade,
tumor size and depth, regional lymph node
involvement and distant metastasis.
Therapy
Histological diagnosis established
Multidisciplinary team to to design most
effective treatment plan
Adjuvant and neoadjuvant chemotherapy
Multimodal protocols
5 years survival rate
Nodular Fasciitis
Self-limiting pseudosarcomatous process
composed of fibroblasts and
myofibroblasts
Most common lesion misdiagnosed as
sarcoma
Rapidly growing, richly cellular with
mitoses
Related to trauma?
Nodular Fasciitis
Signs/Symptoms:
Rapidly growing solitary mass lesion over 1-2
weeks often at site of previous trauma
50% of lesions are painful
Numbness or paresthesia if compression of
peripheral nerve
Age:
Young adults (20-40 years)
Sex:
M = F
Nodular Fasciitis
Anatomic Distribution:
May occur anywhere in the body, though
predilection for upper extremities (volar surface of
forearm), chest wall, back, head & neck and lower
extremities
Hands and feet uncommon
Head & neck most common in children and infants
Nodular Fasciitis
Gross Findings:
Well-circumscribed, non-encapsulated
Most lesions small (< 2.0 cm); lesions up to 10.5
cm have been described
Divided into subcutaneous, intramuscular and
fascial subtypes
Nodular Fasciitis
Microscopic Findings:
Proliferating fibroblasts and myofibroblasts in short
irregular bundles
Reticulin stromal fibrosis
Mitotic activity
Cellular and myxoid areas
Lipid-filled macrophages and giant cells
Nodular Fasciitis
Ancillary Testing:
IHC
Actin positive
Cytokeratin and S100 negative
Prognosis/Treatment:
Benign process
Surgical excision curative
Palmar Fibromatosis
(Dupuytrens Contracture)
Benign fibrous tissue proliferation
More common in Northern Europeans; rare in
Blacks
Genetic component?
Association with unrelated diseases and social
behaviors:
Types I and II DM
Epilepsy
Alcoholism
Hypercholesterolemia
Cigarette smoking
Manual labor
Palmar Fibromatosis
Signs/Symptoms:
Slow growing nodule of hand progression to cord-
like band with contracture of 4
th
or 5
th
digit
Age:
Older adults (20% over 65 years); rare in children
Sex:
M >>> F
Anatomic Distribution:
Palmar surface of hand (R > L)
50% of cases bilateral
Plump immature
fibroblasts with
uniform
appearance and
no mitotic activity
Plump immature
fibroblasts with
uniform
appearance and
no mitotic activity
Palmar Fibromatosis
Ancillary Testing:
N/A
Treatment:
Surgical excision
Recurrence is high unless dermis and fascia are
removed
Abdominal Fibromatosis
(Abdominal Desmoid Tumor)
Locally more aggressive than superficial
fibromatoses
High recurrence rate
Previous trauma
Common in patients with Gardners syndrome
Autosomal dominant
Colonic polyposis
Fundic gland polyps
Soft tissue and bone tumors
Estrogen?
Abdominal Fibromatosis
Signs/Symptoms:
Deep-seated, poorly-circumscribed firm mass in
abdominal wall
Little to no pain
Age:
Young adults (20-30 years)
Sex:
F >>>>>>> M
Gravid or parous females
Anatomic Distribution:
Muscles and fascia of rectus abdominus and internal
oblique
Abdominal Fibromatosis
Gross Findings:
Poorly-circumscribed tumors
Off-white and firm
3-10 cm in diameter
Microscopic Findings:
Proliferating spindle cells in bundles surrounded by
collagen
Limited mitoses
Abdominal Fibromatosis
Ancillary Testing:
N/A
Prognosis/Treatment:
Surgical excision
Recurrence rate 15-30%
Local radiation
Fibrosarcoma
Malignant mesenchymal tumor
Variety of microscopic appearances
Tumors arise from intramuscular and
intermuscular fibrous tissue, fascia,
aponeuroses or tendons
Fibrosarcoma
Signs/Symptoms:
Solitary palpable mass (3.0 to 8.0 cm)
Slow-growing
1/3 of cases present with pain
Age:
Adult-type
30-55 years
Infantile type
First 2 years of life
Congenital
Sex:
M > F
Fibrosarcoma
Anatomic Distribution:
Adult-type
Deep soft tissues of lower extremities
Upper extremities; head & neck
Rare organ involvement (heart, lung, liver, CNS)
Infantile-type
Distal extremities
Gross Findings:
Solitary, lobulated, circumscribed and frequently
encapsulated
May invade adjacent structures
Cellular tumors comprised of fusiform spindle cells
Prominent mitotic activity; little pleomorphism; anaplastic
tumor cells or giant cells are not seen
Fibrosarcoma
Ancillary Testing:
IHC
Vimentin positive
Cytokeratin and S100 negative
Actin variable
Prognosis/Treatment:
Local recurrence rate 50%
Metastasis via bloodstream to lung and bone
5-year survival
Adult-type: 80% for grade 1; 21% for grade 4
Infantile-type: > 80%
Wide surgical excision, RT, chemo
Tumors and Tumor-Like
Conditions of Fibrohistiocytic
Origin
Benign:
Benign Fibrous Histiocytoma (Dermatofibroma)
Intermediate:
Dermatofibrosarcoma Protuberans (DFSP)
Malignant:
Malignant Fibrous Histiocytoma (MFH)
Benign Fibrous Histiocytoma
Signs/Symptoms:
Solitary slow-growing nodule of skin
Often elevated or pedunculated
1/3 of cases multiple
Age:
Young adults to mid-adulthood (20-45 years)
Sex:
M = F
Anatomic Distribution:
Most common on distal extremities
Small red-brown to blue nodules
Poorly-circumscribed, non-encapsulated, cellular
proliferation in dermis; fibroblastic cells arranged in
storiform pattern; numerous foreign body (Touton) giant
cells; Mitoses rare to absent
Benign Fibrous Histiocytoma
Ancillary Testing:
N/A
Prognosis/Treatment:
Simple surgical excision
< 5% recurrence
Dermatofibrosarcoma
Protuberans
Signs/Symptoms:
Slow-growing, non-painful tumor
Antecedent trauma in 10-20% of cases
Age:
Younger than dermatofibroma
Sex:
M > F
Anatomic Distribution:
Trunk, groin and proximal extremities (as opposed
to dermatofibroma)
Solitary masses of subcutis and skin; average size 5.0 cm
May lead to
ulceration of
overlying skin
with associated
hemorrhage and
cystic change
Cellular tumors of
dermis and subcutis;
slender fibroblasts in
monotonous
storiform pattern
Little pleomorphism
with low to moderate
mitotic activity
Dermatofibrosarcoma
Protuberans
Ancillary Testing:
IHC
CD34 positive
Cytogenetics
Supernumerary ring structure formed by amplified
sequences from chromosomes 17 and 22
Fusion of COL1A1 and PDGF genes
Overexpression of PDGF may lead to DFSP
Prognosis/Treatment:
Locally aggressive; recurs in 50% of cases
Rarely metastasizes (<4% of cases)
Wide surgical excision; RT for large tumors or positive
margins
Malignant Fibrous Histiocytoma
Most common sarcoma of late adult life
May occur secondary to previous RT
Signs/Symptoms:
Painless, enlarging mass if on extremity
Retroperitoneal tumors may present with
obstruction and anorexia
Fever and leukocytosis
Tumor production of IL-6, IL-8 and TNF
Age:
Late adulthood (50-70 years)
Sex:
M >> F (70% of MFH in men)
Malignant Fibrous Histiocytoma
Anatomic Distribution:
Lower extremities (thigh), followed by upper
extremities and retroperitoneum
Gross Findings:
Solitary, multilobulated fleshy masses
5-10 cm
Two-thirds within skeletal muscle
Prominent areas of hemorrhage and necrosis
Varied microscopic appearance with pleomorphic tumor cells
Malignant Fibrous Histiocytoma
Ancillary Testing:
> 80% show some cytogenetic abnormality
Prognosis/Treatment:
Local recurrence rate between 19-31%
Metastatic rate between 31-35%
Most common site is lung
Usually within 12-24 months of diagnosis
Treatment by wide radical excision
RT and chemo
Tumors and Tumor-Like
Conditions of Adipose Tissue
Benign:
Lipoma
Malignant:
Liposarcoma
Lipoma
Most common mesenchymal neoplasm
Tumors may be single, multiple, superficial or
deep
Signs/Symptoms:
Painless (except angiolipoma),soft, solitary, mobile
mass
Age:
Adults (40-60 years)
Rare in 1
st
2 decades
Sex:
M > F
Lipoma
Anatomic Distribution:
Upper back, neck, shoulder and abdomen, proximal
extremities, buttocks and upper thigh
Seldom in face,hands or feet
Gross Findings:
Soft, well-circumscribed, thinly-encapsulated rounded
masses
Few millimeters to > 10 cm
Microscopic Findings:
Mature adipose tissue
Many histologic subtypes
Angiolipoma
Spindle cell lipoma
Lipoma
Ancillary Testing:
50-80% have clonal cytogenetic abnormalities with
most common alteration involving translocations of
12q
Prognosis/Treatment:
Simple surgical excision
Recurrence rate < 5%
Liposarcoma
Signs/Symptoms:
Extremity tumors develop as slow-growing masses
Retroperitoneal tumors are associated with abdominal
symptoms
Age:
Late adult life (60-70 years)
Myxoid and round cell subtypes occur in 5
th
decade
Sex:
M = F
Anatomic Distribution:
Deep muscles of extremities or retroperitoneum
Inflammatory
Myxoid
Round Cell
Liposarcoma
Ancillary Testing:
Well-differentiated liposarcomas often possess a giant
ring chromosome (RCG) involving chromosome 12
Myxoid liposarcomas are characterized by
t(12;16)(q13;p11) resulting in fusion of CHOP gene with
TLS gene. CHOP encodes a DNA transcription factor
and TLS encodes an RNA binding protein
Prognosis/Treatment:
Well-differentiated tumors of extremities recur around
50% of time though rarely cause death
Poorly differentiated tumors of retroperitoneum often
recur, metastasize to lung and bone and have a 5-year
survival of 20%
Surgery with chemo and RT
Tumors and Tumor-Like
Conditions of Skeletal Muscle
Malignant
Rhabdomyosarcoma
Rhabdomyosarcoma
Most common soft tissue sarcoma of children
under 15 years of age
Signs/Symptoms:
Tumors in head & neck can present with cranial nerve
signs
Tumors in GU tract present with dysuria, hematuria or
incontinence
Tumors in extremities present as painful, rapidly-growing
masses
Age:
Predominantly infants and children
Sex:
M > F
Rhabdomyosarcoma
Anatomic Distribution:
Head and neck; GU tract and retroperitoneum;
upper and lower extremities
Gross Findings:
Botryoid embyonal tumors of urinary bladder and
nasopharynx present as polypoid masses
comprised of hemorrhagic gelatinous cysts
Tumors of extremities are usually solid and gray-
white
Tumors rarely larger than 3-4 cm
Embryonal
Rhabdomyosarcoma
Alveolar
Rhabdomyosarcoma
Pleomorphic
rhabdomyosarcoma
Rhabdomyosarcoma
Ancillary Testing:
IHC
Desmin and Actin positive
Cytogenetics
Embryonal tumors consistently show LOH at 11p15.5
Alveolar tumors are usually characterized by
t(2;13)(q35;q14) resulting in generation of PAX3-
FKHR chimeric gene which encodes a transcription
factor
Prognosis/Treatment
Prior to 1960, 5-year mortality 100%
Now with surgery, chemo and RT, 5-year survival
for botryoid embryonal rhabdo is 95%; classic
embryonal rhabdo is 66%; alveolar rhabdo is 54%
Metastasis in 20% of cases: lungs, bone, lymph
nodes
Tumors and Tumor-Like
Conditions of Blood Vessels
Benign:
Hemangioma
Malignant:
Angiosarcoma
Hemangioma
Most common benign soft tissue tumor of
infancy and childhood
Signs/Symptoms:
Painless blue or red nodule
Age:
Childhood
Sex:
F > M
Anatomic Distribution:
Predilection for head & neck
Internal tumors of the liver
Hemangioma
Ancillary Testing:
N/A
Prognosis/Treatment:
Surgical excision
INF- for complex or multiple lesions
Hemangiomas do NOT undergo malignant
transformation
Angiosarcoma
Rare
Chronic lymphedema and previous RT
predispose to angiosarcoma
Signs/Symptoms:
Ill-defined bruise with indurated border
Edema, ulceration and necrosis
Age:
Elderly
Sex:
F > M
Anatomic Distribution:
Predilection for skin and superficial soft tissue
Rarely arise from major vessels
Angiosarcoma
Ancillary Testing:
IHC
CD34 and CD31 positive
Cytogenetics
No consistent abnormality
Prognosis/Treatment:
POOR 5-year survival 10-20%
Metastasis to lung, liver, spleen and lymph nodes
Tumors and Tumor-Like Conditions
of Peripheral Nervous Tissue
Benign:
Schwannoma (Neurilemoma)
Neurofibroma
Malignant:
Malignant Peripheral Nerve Sheath Tumor
(MPNST)
Schwannoma
90% of tumors are sporadic
Signs/Symptoms:
Freely mobile, non-painful lesion
Age:
All ages; most common between 20-50 years
Sex:
M = F
Anatomic Distribution:
Head & neck, flexor surfaces of upper and lower
extremities
Schwannoma
Ancillary Testing:
IHC
S100 positive
Prognosis/Treatment:
Simple surgical excision
Neurofibroma
Growth pattern may be localized, diffuse
or plexiform
Diffuse and plexiform tumors occur in the
setting of neurofibromatosis type I (NF1)
aka, von Recklinghausens disease
Localized tumors are sporadic and not
associated with NF1
Neurofibromatosis type 1
1 in every 2500 to 3000 live births
Autosomal dominant with high penetrance
50% of cases are new mutations
Associated with deletions, insertions or mutations of
the NF1 tumor suppressor gene on chromosome 17.
NF1 encodes for neurofibromin
Caf au lait spots; multiple neurofibromas involving
skin, GI tract, larynx, blood vessels and heart
CNS tumors (optic gliomas and astrocytomas)
Asymptomatic pigmentation of iris (Lisch nodules)
Skeletal abnormalities in 40% of cases)
MALIGNANT TRANSFORMATION in a small
percentage of cases (<4%)
Neurofibroma
Signs/Symptoms:
Slow-growing, painless nodules
Age:
Young adults (20-30 years)
Sex:
M = F
Anatomic Distribution:
Dermis throughout the body (internally if NF1)
Neurofibroma
Ancillary Testing:
IHC
S100 positive (to a lesser extent than
schwannoma)
Prognosis/Treatment:
Localized tumors removed by surgical excision
Surgery reserved only for large and painful lesions
in patients with NF1
Malignant Peripheral Nerve Sheath Tumor
25-50% of tumors found in patients with NF1
Signs/Symptoms:
Mass lesion
Age:
20-50 years
Sex:
M = F
Anatomic Distribution:
Most arise in association with major nerve trunks (sciatic
nerve, brachial and sacral plexi)
Gross Findings:
Eccentric masses (> 5 cm) with hemorrhage and
necrosis
Malignant Peripheral Nerve Sheath Tumor
Ancillary Testing:
IHC
S100 variable (weak if present)
Prognosis/Treatment:
Local recurrence rate between 40-60%
5-year survival 50%
Metastasis to bone, lung and pleura
Surgery, chemo and RT
Tumors of Primitive
Neuroectodermal Origin
Malignant:
Extraskeletal Ewings Sarcoma / Primitive
Neuroectodermal Tumor (PNET)
Ewings Sarcoma / PNET
Signs/Symptoms:
Rapidly growing deep-seated masses
Age:
Young adults (usually < 30 years)
Sex:
M > F
Anatomic Distribution:
PNETs usually arise in extremities, upper thigh, buttock
and shoulder
Extraskeletal Ewings sarcoma usually arises in
paravertebral areas in association with vertebrae or ribs
Ewings Sarcoma / PNET
Ancillary Testing:
Cytogenetics
90-95% of tumors are characterized by
t(11;22)(q24;q22) involving EWS on 22q and FLI1 on
11q
Prognosis/Treatment:
Highly aggressive (previously 24 month survival <
25%)
Surgery, chemo and RT
Tumors of Uncertain Type
Malignant:
Synovial Sarcoma
Synovial Sarcoma
Misnomer (occurs in para-articular areas
though has no relation to synovium)
Signs/Symptoms:
Deep-seated, painful mass
Age:
Adolescents and young adults (15-40 years)
Sex:
M > F
Anatomic Distribution:
Extremities (knee, hip and shoulder)
Related to tendons, tendon sheaths and bursae
Rarely reported in nasopharynx, bone and solid
organs
Monophasi
c
Biphasic
Synovial Sarcoma
Ancillary Testing:
IHC
Cytokeratin positive in biphasic tumors
Cytogenetics
Consistent translocation t(X;18)(p11.2;q11.2) in 90%
of tumors involving SYT gene on 18q and SSX gene
on Xp
Prognosis/Treatment:
Metastatic lesions in 50% of patients (lung)
5-year survival 36-82%
Surgery, chemo and RT
Das könnte Ihnen auch gefallen
- Bullous Keratopathy PRDokument12 SeitenBullous Keratopathy PRshevinesaNoch keine Bewertungen
- Kolumna Vertebra: Oleh Gunawan SKMDokument28 SeitenKolumna Vertebra: Oleh Gunawan SKMshevinesaNoch keine Bewertungen
- Patologi Tulang: Dr. Saukani Gumay, Sppa (K)Dokument26 SeitenPatologi Tulang: Dr. Saukani Gumay, Sppa (K)shevinesaNoch keine Bewertungen
- Anestesi Lokal Pada Lesi Superfisial: Huntal NapoleonDokument12 SeitenAnestesi Lokal Pada Lesi Superfisial: Huntal NapoleonshevinesaNoch keine Bewertungen
- Tuberculosis, Bronchiectasis and Chronic Airflow ObstructionDokument6 SeitenTuberculosis, Bronchiectasis and Chronic Airflow ObstructionshevinesaNoch keine Bewertungen
- Bronchiectasis New ZealandDokument4 SeitenBronchiectasis New ZealandshevinesaNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- KDIGO 2023 CKD Guideline Public Review Draft 5 July 2023Dokument339 SeitenKDIGO 2023 CKD Guideline Public Review Draft 5 July 2023oscar coreaNoch keine Bewertungen
- CHDC8 Cargador de BateriasDokument1 SeiteCHDC8 Cargador de Bateriasleoscalor6356Noch keine Bewertungen
- Deviance, Crime, and Social ControlDokument17 SeitenDeviance, Crime, and Social ControlSaad MaqboolNoch keine Bewertungen
- A Sound of Thunder - Ray BradburyDokument9 SeitenA Sound of Thunder - Ray BradburyBrenden CheeNoch keine Bewertungen
- Assignment 4Dokument4 SeitenAssignment 4ShabihNoch keine Bewertungen
- Real Time EvaluationDokument3 SeitenReal Time Evaluationأيوب علاءNoch keine Bewertungen
- Acc030 Financial Statement & Income Statement FormatDokument2 SeitenAcc030 Financial Statement & Income Statement FormatAqilahNoch keine Bewertungen
- Composition and Digestibility of Cattle Fecal WasteDokument7 SeitenComposition and Digestibility of Cattle Fecal WasteIonela HoteaNoch keine Bewertungen
- 7-13-1996 Joel Nance MDDokument3 Seiten7-13-1996 Joel Nance MDAnother AnonymomsNoch keine Bewertungen
- CV TemplateDokument5 SeitenCV TemplateLopezDistrict FarmersHospitalNoch keine Bewertungen
- Fischer General-CatalogueDokument108 SeitenFischer General-Cataloguebo cephusNoch keine Bewertungen
- TOCDokument14 SeitenTOCAthirah HattaNoch keine Bewertungen
- Bar Exam Questions Week 1Dokument30 SeitenBar Exam Questions Week 1Mark Bantigue100% (1)
- Evaluation and Comparison of Highly Soluble Sodium Stearyl Fumarate With Other Lubricants in VitroDokument8 SeitenEvaluation and Comparison of Highly Soluble Sodium Stearyl Fumarate With Other Lubricants in VitroSvirskaitė LaurynaNoch keine Bewertungen
- General Leasing and Managing AuthorityDokument14 SeitenGeneral Leasing and Managing AuthorityKatharina SumantriNoch keine Bewertungen
- D435L09 Dental Trauma-2C Cracked Teeth - 26 Root FractureDokument73 SeitenD435L09 Dental Trauma-2C Cracked Teeth - 26 Root FractureD YasIr MussaNoch keine Bewertungen
- Field Study 1-Act 5.1Dokument5 SeitenField Study 1-Act 5.1Mariya QuedzNoch keine Bewertungen
- High Pressure Processing of Food - Principles, Technology and ApplicationsDokument758 SeitenHigh Pressure Processing of Food - Principles, Technology and ApplicationsEduardo Estrada100% (1)
- War RoomDokument88 SeitenWar RoomDada Sasa100% (1)
- Mechanical Interview Questions and Answers - Fluid MechanicsDokument2 SeitenMechanical Interview Questions and Answers - Fluid MechanicsannukiitNoch keine Bewertungen
- Standard DetailsDokument168 SeitenStandard DetailsMurathan Paksoy100% (1)
- Cystostomy NewDokument32 SeitenCystostomy Newkuncupcupu1368Noch keine Bewertungen
- Science Grade 7: Active Reading Note-Taking GuideDokument140 SeitenScience Grade 7: Active Reading Note-Taking Guideurker100% (1)
- National Federation OF Sugar Workers (NFSW), Petitioner, vs. ETHELWOLDO R. OVEJERA Et. Al., RespondentsDokument32 SeitenNational Federation OF Sugar Workers (NFSW), Petitioner, vs. ETHELWOLDO R. OVEJERA Et. Al., RespondentsRon GawatNoch keine Bewertungen
- Leadership Roles and Management Functions in Nursing Theory and ApplicationDokument2 SeitenLeadership Roles and Management Functions in Nursing Theory and Applicationivan0% (3)
- Homoeopathic Treatment of Complicated Sebaceous Cyst - A Case StudyDokument5 SeitenHomoeopathic Treatment of Complicated Sebaceous Cyst - A Case StudyDr deepakNoch keine Bewertungen
- Boost Listening 1 Teacher S Edition PDFDokument96 SeitenBoost Listening 1 Teacher S Edition PDFHuy Lê QuangNoch keine Bewertungen
- Blood Anatomy and Physiology ReviewDokument20 SeitenBlood Anatomy and Physiology ReviewStacey CamilleNoch keine Bewertungen
- Arc Welding Rod Chart byDokument1 SeiteArc Welding Rod Chart bytayyab aliNoch keine Bewertungen
- Membrane AutopsyDokument2 SeitenMembrane AutopsyBiljana TausanovicNoch keine Bewertungen