Beruflich Dokumente
Kultur Dokumente
Tuberculosis 140515184439 Phpapp01
Hochgeladen von
Veronica Wong Huey ShinCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Tuberculosis 140515184439 Phpapp01
Hochgeladen von
Veronica Wong Huey ShinCopyright:
Verfügbare Formate
PATHOGENESIS OF TUBERCULOSIS
Dr. Mohamed Zakaria Sayed-Ahmed
Assistant Prof. of Infectious Diseases
2014
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
TUBERCULOSIS (TB)
Is the most prevalent communicable infectious disease
on earth and remains out of control in many
developing nations
It is a chronic specific inflammatory infectious disease
caused by Mycobacterium tuberculosis in humans
Usually attacks the lungs but it can also affect any parts
of the body
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
TUBERCULOSIS (TB)
Coinfection with HIV
o Accelerates the progression of both diseases
o Requiring rapid diagnosis and treatment of both diseases
Tuberculosis can produce atypical signs and symptoms in
infants, the elderly, and immunocompromised hosts
and it can progress rapidly in these patients
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
ETIOLOGY
Mycobacterium tuberculosis
It presents either as latent TB infection (LTBI) or as progressive
active disease.
The latter typically causes progressive destruction of the lungs, leading
to death in most patients who do not receive treatment
Common cause other than tuberculosis includes:
o M. avium intracellulare, M. scrofulaceum
o M. ulcerans, M. fortuitum, etc.
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
EPIDEMIOLOGY
Roughly one of every three people on earth is infected by
M. tuberculosis (WHO, 2008)
The distribution is very uneven, with the highest incidences
found in southern Asia and sub-Saharan Africa
In the United States, about 13 million people have LTBI,
evidenced by a positive skin test [puried protein derivative
(PPD)] but no signs or symptoms of disease
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
EPIDEMIOLOGY
Every year approximately 1.7 million people develop TB
Tuberculosis (TB) kills about 2 million people each year
With the spread of AIDS, tuberculosis continues to lay waste to
large populations
The emergence of drug resistant organism threatens to make this
disease once again incurable
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
RISK FACTORS OF TUBERCULOSIS
Low socioeconomic status
Crowded living conditions
Diseases that weakens immune system like HIV
Person on immunosuppresants like steroid Health care workers
Migration from a country with a high number of cases
Alcoholism
Recent Tubercular infection (within last 2 years)
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
COINFECTION WITH HUMAN
IMMUNODEFICIENCY VIRUS (HIV)
HIV is the most important risk factor for active TB, because
the immune decit prevents patients from containing the initial
infection
Roughly 10% of US TB patients are coinfected with HIV, and
roughly 20% of TB patients ages 25 to 44 years are coinfected
with HIV
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
SITES INVOLVED
Pulmonary TB (85% of all TB cases)
Brain
Bone
Extra-pulmonary sites
Lymph node
Genito-urinary tract
Bones & Joints
Meninges
Intestine
Skin
Larynx
Lymph
node
Lung
Spine
Kidney
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
CHARECTERISTICS OF M. TUBERCULOSIS
Rod shaped,
0.2-0.5 in D, 2-4 in L
Mycolic acid present in its cell
wall, makes it acid fast
It resists decolourization with
acid & alcohol
Aerobic and non motile
It multiplies slowly, can remain dormant for decades
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
How is TB Transmitted?
Person-to-person through the
air by a person with active TB
Droplet nuclei
containig tubercle
baccilli
disease of the lungs
Less frequently transmitted by:
Ingestion of M. bovis
found in unpasteurized milk
Inoculation (in skin tuberculosis)
Transplacental route (rare route)
Tubercle bacilli
multiply in the alveoli
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Primary Infection
The progression to clinical disease in a previously unexposed,
immunocompetent person depends on three factors:
(1) The number of M. tuberculosis organisms inhaled
(2) Infecting dose and the virulence of these organisms
(3) The development of anti-mycobacterial cell-mediated
immunity
Immunity to M. tuberculosis is primarily mediated by TH1 cells,
which stimulate macrophages to kill the bacteria
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Disease that develops in a previously
unexposed person. Almost always begins in
lungs
Inhaled bacilli implant in the distal airspaces
of lower part of upper lobe or upper part of
lower lobe
1-1.5 cm area of grey white inflammation
with consoldation develops, called as
Ghon focus which often caseates
Parenchymal lung lesion + Lnns involvement = Ghons complex
Ghons complex: Subpleural granuloma at right along
with Granuloma in the hilar lymph node
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Disease that develops in a previously
unexposed person. Almost always begins in
lungs
Inhaled bacilli implant in the distal airspaces
of lower part of upper lobe or upper part of
lower lobe
1-1.5 cm area of grey white inflammation
with consoldation develops, called as
Ghon focus which often caseates
Parenchymal lung lesion + Lnns involvement = Ghons complex
Ghons complex: Subpleural granuloma at right along
with Granuloma in the hilar lymph node
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
1. M. tuberculosis enters macrophages by endocytosis mediated by several macrophage receptors:
mannose receptors bind lipoarabinomannan, a glycolipid in the bacterial cell wall
2. Inside the macrophage, M. tuberculosis replicates within the phagosome by blocking phaglysosome formation
Inhibition of Ca2+ signals
and blocking recruitment
Assembly of the proteins
which mediate
phagosome-lysosome
fusion
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
1. About 3 weeks after infection, a TH1 response against M. tuberculosis is mounted that activates
macrophages to become bactericidal.
2.
Differentiation of TH1 cells depends on the presence of IL-12, which is produced by antigen presenting cells
3. Mature TH1 cells, both in
lymph nodes and lung, produce
IFN-. IFN- is the critical
mediator which drives
macrophages to become
competent to contain the M.
tuberculosis infection.
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Histopathological changes
Granulomatous inflammation forms both caseating
and non caseating tubercles
Tuberculous granuloma has the following criteria:
1.
2.
3.
4.
Rounded outlines
Central caseous necrosis
Transformed macrophages called epithelioid cells
Lymphocytes, plasma cells, and fibroblasts
Tubercle bacilli
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Central
caseated
necrosis
Giant multinucleated
cells (langhans type
Agrregation
of epithliod
cells
Collar of
lymphocytes,
plasma cells
Well-defined granulomas . They have rounded outlines. The center contains
several Langhans giant cells. Granulomas are composed of transformed
macrophages called epithelioid cells along with lymphocytes, plasma cells, and
fibroblasts. The localized, small appearance of these granulomas suggests that
the immune response is fairly good
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
PRIMARY TUBERCULOSIS
Occasionally, even in immunocompetent
individuals, tubercular granulomas might
not show central caseation
In immunosuppressed individuals, tuberculosis may
not elicit a granulomatous response ("nonreactive
tuberculosis"); instead, sheets of foamy histiocytes are
seen, packed with mycobacteria that are demonstrable
with acid-fast stains
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
FATE OF PRIMARY TUBERCULOSIS
No progression
Healing by fibrosis and calcification
Ghons complex after undergoing progressive
fibrosis produces radiologically detectable
calcification called as Ranke complex
Progressive primary tuberculosis
Primary miliary tuberculosis
Tubercle bacilli escape
and multiply
Dissemination to organs like liver, spleen, kidney, ..etc.
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
SECONDARY PULMONARY TUBERCULOSIS
The upper parts of both lungs Showed:
Gray-white areas of caseation
Multiple areas of softening and cavitation
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
FATE OF SEC. PULMONARY TUBERCULOSIS
The lesion may heal with fibrous scarring and calcification
The lesions may coalesce together to form large area of
tuberculous pneumonia and produce progressive secondary
pulmonary tuberculosis producing pulmonary & extra pulmonary
lesions:
Tuberculous caseous pneumonia
Fibrocaseous tuberculosis
Miliary tuberculosis
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
MILIARY TUBERCULOSIS
Extensive infection via hematogenous spread
In lung: lesions are either microscopic or small, visible foci (2mm) of
yellow white consolidation scattered through out lung parenchyma
Miliary pulmonary disease can cause pleural effusion, tuberculous
empyema or obliterative fibrous pleuritis.
Extra pulmonary miliary tuberculosis is most prominent in the
liver, spleen, bone marrow, adrenals, meninges, kidneys, fallopian
tubes and epididymis but can involve any organ
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
MILIARY TUBERCULOSIS
Miliary tuberculosis of the spleen
The cut surface shows numerous gray-white granulomas
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
EXTRA PULMONARY TUBERCULOSIS
In tissues or organs seeded hematogenously
Commonly involved organs include:
Intestinal tuberculosis (Primary, Secondary and hyperplastic)
Meninges (Tuberculous meningitis)
Kidneys (Renal tuberculosis)
Adrenals (Addison disease)
Bones (Osteomyelitis)
Vertebrae (Pott disease)
Fallopian tubes (Salpingitis)
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
Inuence of HIV Infection on Pathogenesis
HIV infection is the most important risk factor for active TB.
As CD4+ lymphocytes multiply in response to the
mycobacterial infection, HIV multiplies within these cells and
selectively destroys them, gradually eliminating the TB-ghting
lymphocytes
HIV-infected patients infected with TB are at a substantially higher
risk of early mortality compared with HIV-negative TB patients
Most clinicians elect to begin TB treatment rst. A reasonable time to
begin HIV treatment is after 2 months of TB treatment
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
CLINICAL Findings
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
CLINICAL PRESENTATION OF TUBERCULOSIS
Signs and Symptoms
Patients typically present with weight loss, fatigue, a productive
cough, fever, and night sweats
Physical Examination
Dullness to chest percussion, rales
Auscultation revealed vocal fremitus sound
Laboratory Tests
Moderate elevations in the white blood cell (WBC) count
with a lymphocyte predominance
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
CLINICAL PRESENTATION OF TUBERCULOSIS
Chest Radiograph:
Patchy or nodular infiltrates in the apical areas of the upper lobes
or the superior segment of the lower lobes
Cavitation that may show air-fluid levels as the
infection progresses
CT scan: To diagnose TB that has spread throughout the body
(miliary TB) and to detect lung cavities caused by TB
MRI: This test looks for TB in the brain or the spine
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
Chest radiographs in pulmonary tuberculosis
A. Infiltrates in left lung
B. Ghons complex (Primary tuberculosis)
C. Bilateral advanced pulmonary tuberculosis and cavitation in apical area of right lung
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
People Exposed to M. tuberculosis
No
Negative TST* or
IGRA** result
No developed
LTBI or TB
Infected
with M.
tuberculosi
s
Ye
s
Normal chest
radiograph
No symptoms
No Infection
Has LTBI
No active infection
* TST (Tuberculin skin test)
* IGRA (Interferon-Gamma
Release Assays)
Develop symptoms later
Positive TST or
IGRA result
abnormal chest
radiograph
symptoms
Positive culture
Has TB Disease
May be infectious
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
DIAGNOSIS
SKIN TESTING
Infection with M. tuberculosis typically leads to the development
of delayed hypersensitivity to M. tuberculosis antigens, which can
be detected by the tuberculin (Mantoux) test
About 2 to 4 weeks after infection, intracutaneous injection of
purified protein derivative of M. tuberculosis (PPD) induces a
visible and palpable induration that peaks in 48 to 72 hours
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
DIAGNOSIS
A positive tuberculin test result signifies cell-mediated
hypersensitivity to tubercular antigens. It does not differentiate
between infection and disease
False-negative reactions may be produced by certain viral infections,
sarcoidosis, malnutrition, immunosuppression
False-positive reactions may also result from infection by atypical
mycobacteria
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
DIAGNOSIS
Sputum examination
Are essential to confirm TB Best collected in morning before any meal
Sputum examination on 3 days, increase chances of detection
Sputum can be collected from laryngeal swab or bronchial washing In
small children, gastric lavage can be examined.
Smear should be prepared from thick dirty part of sputum & stained
with Ziehl-Neelson technique
.
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
TREATING TB DISEASE (GENERAL PRINCIPLES)
Always treat with multiple drugs. Never add a single drug to a
failing regimen.
Treatment course depends on the categories of the patient
Usually 6 months, sometimes 9 months
Four drugs for two months Isoniazid Rifampicin Ethambutol Pyrazinamide
Two drugs for four or seven months Isoniazid - Rifampicin
DOTS (Directly Observed Treatment Short-course ) is given
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
TREATING LATENT INFECTION
Isoniazid is the preferred drug for treating latent TB infection
Generally, isoniazid alone is given for 9 months for latent
TB infection (LTBI) reduces a persons lifetime risk of active TB
Pathogenesis of Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis References
REFERENCES
1.
Charles A. Peloquin. Tuberculosis. In: Pharmacotherapy: A Pathophysiologic Approach, 7th ed. Dipiro JT,
Talbert RL, Yee GC, et al., eds. New York: McGraw-Hill; 2008:18391856.
2.
Charles A. Peloquin. Tuberculosis. In: Pharmacotherapy: Principle & Practice, 7th ed. Dipiro JT,
Talbert RL, Yee GC, et al., eds. New York: McGraw-Hill.
3.
Cotran RS, Kumar V, Collins T. Tuberculosis. In: Cotran RS, Kumar V, Collins T, 7th eds. Robbins
Pathologic Basis of Disease. Philadelphia: WB Saunders, 1999: 260328.
4. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings,
2005.
MMWR 2005; 54 (No. RR-17). www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm?s_cid=rr5417a1_e
5.World Health Organization Report on the Global Tuberculosis Epidemic. Geneva: WHO, 2008.
6.Pathology and therapeutics for pharmacist: A B for clinical pharmacy practice-Green and Harris,
Chapman and hall publication.
Thank you for your attention
BACK-UP SLIDES
Tuberculosis
Introduction Etiology Epidemiology Pathophysiology Clinical features Diagnosis Treatment
TUBERCULOUS CASEOUS PNEUMONIA
The caseous material from a case of secondary tuberculosis in an
individual with high degree of hypersensitivity, may spread to rest of
the lung producing caseous pneumonia.
FIBROCASEOUS TUBERCULOSIS
The original area of Tuberculous pneumonia undergoes massive central
caseation necrosis which may-Break in to a bronchus forming a cavity
called as Cavitary or Open Fibrocaseous TB
and become the source of spread of infection to others (open
tuberculosis).
It can lead to endobronchial and endotracheal TB.
Remain as a soft caseous lesion without drainage in to a bronchus or
bronchiole to produce a non cavitary lesion called as Chronic Fibrocaseous
TB.
Tuberculosis
Introduction
Etiology
Epidemiology
Pathogenesis
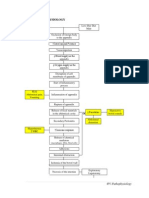
PATHOGENESIS OF TUBERCULOSIS
M.Tuberculosis
Aggregation of
macrophage
(Tubercle form)
capsule
Fibrous
eated
and cas
center
T-lymphocyte
mediated reaction
(Tissue damage)
Aersols,
Ingestion
Local Lns
(Primary complex)
Macrop
hage k
some T illed
B
With or without
calcification and
liquification
Contagious
extension via blood
vessels to bronchi
and viscera
ek
1st we
Blood generalized
TB
(miliary TB)
Tuberculosis
Introduction
Etiology
Epidemiology
Pathophysiology
INTESTINAL TUBERCULOSIS
Occurs in three forms
1. Primary intestinal tuberculosis : Used to occur by ingestion of
unpasteurised cows milk infected with Mycobacterium bovis. But now a
days most cases are due to M. tuberculosis.
Most commonly ileocaecal region is involved.
Subsequently, mesentric lymph nodes are affected which show typical
tuberculous granulomatous inflammatory reaction with caseation
necrosis
Tuberculosis
Introduction
Etiology
Epidemiology
Pathophysiology
INTESTINAL TUBERCULOSIS
2. Secondary intestinal tuberculosis:
Swallowing of sputum in patients with active pulmonary tuberculosis
may cause secondary intestinal tuberculosis.
Most commonly in the terminal ileum and rarely in the colon.
Histologically: tubercles will be present.
Mucosa and submocosa show ulceration and the muscularis may be
replaced by variable degree of tuberculosis.
3. Hyperplastic intestinal tuberculosis : The caecum and ascending
colon are thick walled with mucosal ulceration. Histologically: caseating
tubercles will be present.
Tuberculosis
Introduction
Etiology
Epidemiology
Pathophysiology
INTESTINAL TUBERCULOSIS
2. Secondary intestinal tuberculosis:
Swallowing of sputum in patients with active pulmonary tuberculosis
may cause secondary intestinal tuberculosis.
Most commonly in the terminal ileum and rarely in the colon.
Histologically: tubercles will be present.
Mucosa and submocosa show ulceration and the muscularis may be
replaced by variable degree of tuberculosis.
3. Hyperplastic intestinal tuberculosis : The caecum and ascending
colon are thick walled with mucosal ulceration. Histologically: caseating
tubercles will be present.
Tuberculosis
Introduction
Etiology
Epidemiology
Pathophysiology
CUTANEOUS TUBERCULOSIS
Cutaneous tuberculosis has various clinical and morphological forms
depending on the mode of entry and whether it is primary or
secondary infection.
LUPUS VULGARIS : It is reactivation type of tuberculosis. Generally
involves the face and the lesions are formed of red patches in which
small, firm nodules reside.
Microscopically, non necrotic and less commonly necrotic
granulomas are found in the dermis.
DOTS (directly observed treatment, short-course), is the
name given to the tuberculosis control strategy recommended by
the World Health Organization.[1] According to WHO, The most
cost-effective way to stop the spread of TB in communities with a
high incidence is by curing it. The best curative method for TB is
known as DOTS.[2] DOTS has five main components:
Government commitment (including political will at all levels, and
establishment of a centralized and prioritized system of TB
monitoring, recording and training).
Case detection by sputum smear microscopy.
Standardized treatment regimen directly of six to eight months
observed by a healthcare worker or community health worker for
at least the first two months.
A regular, uninterrupted drug supply.
A standardized recording and reporting system that allows
assessment of treatment results.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Zika VirusDokument25 SeitenZika VirusSumit Sharma PoudelNoch keine Bewertungen
- Cranial Base ScottDokument30 SeitenCranial Base ScottShirley AliagaNoch keine Bewertungen
- Sychology Actsheets: The Biological Approach To PsychologyDokument5 SeitenSychology Actsheets: The Biological Approach To PsychologyAyse Kerim100% (1)
- Farmakodinamik Nsaid 2018Dokument57 SeitenFarmakodinamik Nsaid 2018kiki rawitriNoch keine Bewertungen
- Antifungal AgentsDokument16 SeitenAntifungal AgentstheintrovNoch keine Bewertungen
- Diagnostic Test For Endocrine DisordersDokument4 SeitenDiagnostic Test For Endocrine DisordersjesperdomincilbayauaNoch keine Bewertungen
- Modern Pediatric Dentistry PDFDokument14 SeitenModern Pediatric Dentistry PDFsana alia0% (1)
- Chapter 38 Animal DevelopmentDokument77 SeitenChapter 38 Animal Developmentmaria banunaekNoch keine Bewertungen
- Basics On Test Selection For Parasites in The CatDokument4 SeitenBasics On Test Selection For Parasites in The CatChantelle NeufeldNoch keine Bewertungen
- Anatomy and Physiology of NoseDokument32 SeitenAnatomy and Physiology of NoseBinita ShakyaNoch keine Bewertungen
- Case Study Pleural EffusionDokument32 SeitenCase Study Pleural Effusionwguino100% (1)
- Practicing Adverb Clauses AnswersDokument9 SeitenPracticing Adverb Clauses Answersasvas100% (1)
- SD - Cauda Equina InglesDokument20 SeitenSD - Cauda Equina InglesRodriguezNoch keine Bewertungen
- PBL Report Traumatology: Group 6Dokument42 SeitenPBL Report Traumatology: Group 6anthy putrisriyantiNoch keine Bewertungen
- Pms QuestDokument2 SeitenPms QuestsandracassssNoch keine Bewertungen
- Nervous System Concept MapDokument12 SeitenNervous System Concept MapJo BrackenNoch keine Bewertungen
- Cloning PresentationDokument75 SeitenCloning PresentationGerwyn Gervacio C100% (4)
- CR DR - Dedi Hidropneumothorax Ec TB ParuDokument38 SeitenCR DR - Dedi Hidropneumothorax Ec TB ParuBunga Listia ParamitaNoch keine Bewertungen
- Whybatsflyonlyatnight CLRDokument7 SeitenWhybatsflyonlyatnight CLRRaj ManoNoch keine Bewertungen
- Acupuncture ChartsDokument7 SeitenAcupuncture Chartsdoringrama50% (2)
- Efficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsDokument3 SeitenEfficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsAmit Kumar PandeyNoch keine Bewertungen
- CurosurDokument2 SeitenCurosuredNoch keine Bewertungen
- Poecilia Reticulata Domestic Breeder Tra PDFDokument18 SeitenPoecilia Reticulata Domestic Breeder Tra PDFAdrian BercanNoch keine Bewertungen
- Appendicitis PathophysiologyDokument4 SeitenAppendicitis PathophysiologyAngelica Cassandra VillenaNoch keine Bewertungen
- AmphiprioninaeDokument7 SeitenAmphiprioninaestevenspillkumarNoch keine Bewertungen
- Fecal IncontinenceDokument57 SeitenFecal Incontinenceiqiqiqiqiq100% (1)
- Word Parts Dictionary ADokument27 SeitenWord Parts Dictionary AJosh Flynn100% (1)
- Bio 205 Lab Final Study GuideDokument8 SeitenBio 205 Lab Final Study GuideJames DuongNoch keine Bewertungen
- Antonio Damasio, Hanna Damasio - Fear and The Human AmigdalaDokument13 SeitenAntonio Damasio, Hanna Damasio - Fear and The Human AmigdalaAna Victoria Casillas ZapataNoch keine Bewertungen
- Head To Toe Assessment 1Dokument2 SeitenHead To Toe Assessment 1Monica Ugarte Treta100% (4)