Beruflich Dokumente
Kultur Dokumente
Clinical Pharmacist in ICU
Hochgeladen von
ApriyanCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Clinical Pharmacist in ICU
Hochgeladen von
ApriyanCopyright:
Verfügbare Formate
Role of the Clinical
Pharmacist in Intensive
Care: Review of the
Evidence
Adnan Hajjiah
Critical Care Pharmacist
MSc Clinical Pharmacy, MPharm
Mubarak Al-Kabeer Hospital
Why the need for a clinical
?pharmacist in intensive care settings
Critically ill patients often have multisystem organ failure
Multisystem organ failure along with polypharmacy predispose to
medication toxicities
Co-morbidities, altered drug pharmacokinetics and drug-drug
interactions further enhance the risk for both overdosing and
underdosing and adverse medication events including acute kidney
injury, hepatotoxicity, neurological dysfunction and other end-organ
disturbances
Why the need for a clinical
?pharmacist in intensive care settings
The dynamic nature of intensive care units involving healthcare
professionals with different experiences and backgrounds allows for
great variability in patient care
Protocol development driven by clinical pharmacists can positively
impact such variability
Clinical pharmacy services
The profession of pharmacy has evolved over the past 50 years from
focusing solely on pharmaceutical products into a discipline that is more
patient-centered with special attention to optimal delivery of
pharmaceutical care
Curricula in most pharmacy colleges have changed significantly to
include courses in pharmacotherapeutics, pharmacokinetics,
pathophysiology, and Pharmacoeconomics to prepare graduates for
careers as clinicians
Evolution of critical care pharmacy
Clinical pharmacy services in critical care settings have expanded
dramatically and include assisting physicians in pharmacotherapy
decision making, providing pharmacokinetic consultations, monitoring
patients for efficacy and safety and providing drug information
During the 1980s, critical care pharmacists designed specialized training
programs and increased participation in critical care organizations
followed by developing standards for critical care residency
Several professional pharmacy organizations formed specialty groups
consisting of critical care pharmacists including: the American College of
Clinical Pharmacy and American Society of Health-System Pharmacists
Evolution of critical care pharmacy
In 1989, the Society of Critical Care Medicine acknowledged the
necessity and value of pharmacists as members of physician-led
multidisciplinary team
In 2000, the SCCM along with ACCP developed a position paper that
stratified clinical pharmacy services into three levels; namely
fundamental, desired and optimal services
Clinical Pharmacy Services
in Intensive Care
Numerous research articles have identified areas in which critical care
pharmacists make significant contributions to patient care
Most of this literature describes the responsibilities of these pharmacists as
follows:
Drug-use evaluation
Drug error management
In-service education
Pharmacokinetic consultations
Drug therapy monitoring
Written drug histories
Written documentation in medical records
Other activities
Therapeutic drug monitoring
Participation in patient care rounds
Prevention of drug-drug interactions
Prevention, minimization and management of ADRs
Provision of drug information and therapeutic consultation
Reduction in medication costs
Education of ICU professionals regarding drug-related aspects
Education of nursing staff for optimal administration/reconstitution
Development of medication protocols and policies to minimize errors and
improve outcomes
The evidence
Impact of clinical pharmacist in a
cardiac-surgery intensive care unit
Dec 2002 to May 2003
19-bed cardiac-surgery ICU at King Faisal Specialist Hospital and
Research Centre, Riyadh
The clinical pharmacist made 394 interventions (94% success rate)
No medication prescribed for medical condition (33%)
Inappropriate dosing regimen (28%)
No indication for use (14%)
Saudi Medical Journal 2008, Al-Jazairi AS et al.
Impact of clinical pharmacistenforced sedation protocol on
mechanical ventilation and hospital
stay
Before-after study (18 bed medical ICU)
Mean duration of mechanical ventilation reduced from 14 days to 7.4
days in the post-intervention group (p < 0.001)
Duration of both ICU and hospital stays were also significantly reduced
in the post-intervention group
Critical Care Medicine 2008, Marshall J.
Impact on preventable adverse drug
events (1)
Before-after comparison study
Medical ICU (study unit), CCU (control)
A senior pharmacist made rounds with the ICU team in the morning and was
available on call throughout the day
Within 9 months, the rate of preventable ADEs decreased by 66% from 10.4
per 1000 patient-days before the intervention to 3.5 following the intervention
In the control groups, rate remained unchanged
366 recommendations were made by the pharmacists with 99% acceptance
rate
Journal of American Medical Association 1999, Leape LL et al.
Impact on preventable adverse drug
events (2)
Intervention study
8.5 months in an adult medical and surgical ICU, the Netherlands
ICU hospital pharmacist made a total of 659 recommendations with consensus
rate of 74% between the pharmacist and physicians
Incidence of prescribing errors during intervention period was significantly lower
than baseline (62.5 per 1000 monitored patient-days versus 190.5 per 1000
monitored patient-days, p < 0.0001)
Preventable ADEs were reduced from 4.0 per 1000 monitored patient-days
during baseline period to 1.0 per 1000 monitored patients-days during the
intervention period (p = 0.25)
Critical Care 2010, Klopotowska JE et al.
Impact on drug therapy costs (1)
Tertiary care teaching hospital
Over a 7 month period
117 recommendations were made (94% acceptance rate)
Total net cost savings was USD 1796.73
Journal of Pharmacology and Pharmacotherapeutics 2012, Lucca JM et al.
Impact on drug therapy costs (2)
Before-after comparative study
Al-Hussein Hospitals ICU, Jordan
10 months period
Total reduction of drug therapy costs was USD 211574.9 representing an
average of 35.8% reduction when compared to the first period
Saudi Pharmaceutical Journal 2013, Aljbouri TM, et al.
Impact on drug therapy costs (3)
Intervention study
Surgical ICU
Over 4.5 months
A total of 129 interventions were documented
Potential cost avoidance of documented interventions was USD 209,919
280,421
American Journal of Health-System Pharmacy 2007, Kopp BJ et al.
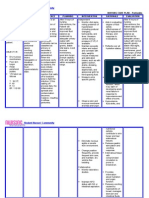
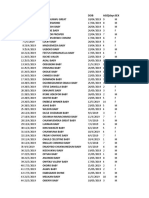
Interventions In Mubarak AlKabeer Hospital Intensive
Care Unit
Interventions made
In a random 52-week period, a total of 243 successful interventions were
made
Percentage of dose and frequency adjustments consisted of 40% of the
total number of interventions
Percentage of pharmaceutical consultation 54%
Medication reviews and reconciliation 6%
Interventions made (contd)
Interventions involving antibiotic therapy (including choice, dose,
frequency, monitoring and duration of treatment) accounted for 30% of
all interventions
Antihypertensives and antifungals accounted for 10% of total
interventions (choice, dose adjustments and switching between oral and
intravenous formulations)
Recommendations
Establishment of specialized clinical pharmacy programs in intensive
care settings in collaboration between intensive care professionals and
the pharmacy department
Participation of dedicated pharmacists preferably with postgraduate
training in clinical pharmacy services
Summary
Critical care pharmacists are crucial members in the ICU
multidisciplinary team
Provided with adequate training, critical care pharmacists can reduce
prescribing errors, preventable ADEs and medication costs with potential
improvement in patient outcomes
Das könnte Ihnen auch gefallen
- DR - Khan Clinical Pharmacy OrientationDokument55 SeitenDR - Khan Clinical Pharmacy OrientationIram CHNoch keine Bewertungen
- Phm423: Clinical Pharmacy Week 1: Introduction: Hadassah M. Reyes-Cendana, RPH January 2022Dokument36 SeitenPhm423: Clinical Pharmacy Week 1: Introduction: Hadassah M. Reyes-Cendana, RPH January 2022Hadassah ReyesNoch keine Bewertungen
- 1 Introduction Clinical Pharmacy 2Dokument54 Seiten1 Introduction Clinical Pharmacy 2Sajid Hassan GhafoorNoch keine Bewertungen
- Clinical PharmacyDokument38 SeitenClinical PharmacyJurusan Farmasi Poltekkes MedanNoch keine Bewertungen
- ASHP Critical Care Pharmacy Specialty Review and Recertification CourseDokument16 SeitenASHP Critical Care Pharmacy Specialty Review and Recertification Courseap2187cpNoch keine Bewertungen
- Medication Errors: P AperDokument4 SeitenMedication Errors: P Aperdesk ayu okaNoch keine Bewertungen
- 18 WB - CC - Practice - Adminstration - and - Development - Pharmacoeconomics - and - Safe - Medication - UseDokument36 Seiten18 WB - CC - Practice - Adminstration - and - Development - Pharmacoeconomics - and - Safe - Medication - UsekushishaNoch keine Bewertungen
- ACCP Farmakoterapi 2013Dokument296 SeitenACCP Farmakoterapi 2013Decy RahmawatiNoch keine Bewertungen
- 1.2 PharmacotherapyDokument25 Seiten1.2 PharmacotherapyAmina Akther Mim 1821179649Noch keine Bewertungen
- 2017 Critical Care Pharmacy Drug Guideline Folder PDFDokument182 Seiten2017 Critical Care Pharmacy Drug Guideline Folder PDFDeniNoch keine Bewertungen
- Glucose Management and Insulin Treatment in Intensive CareVon EverandGlucose Management and Insulin Treatment in Intensive CareNoch keine Bewertungen
- Statements Pharmaceutical CareDokument3 SeitenStatements Pharmaceutical CareDiegoAndrésYiZapataNoch keine Bewertungen
- Pharmaceutical Care Process 2017Dokument22 SeitenPharmaceutical Care Process 2017ChristinaNoch keine Bewertungen
- Pharmaceutical CareDokument27 SeitenPharmaceutical Caremai elewaNoch keine Bewertungen
- Basic - Concepts - in - Pharmaceutical - Care CLINICAL PHARMACYDokument17 SeitenBasic - Concepts - in - Pharmaceutical - Care CLINICAL PHARMACYPrincess RonsableNoch keine Bewertungen
- NHS Lothian Pharmacy Strategy 2013-2016Dokument28 SeitenNHS Lothian Pharmacy Strategy 2013-2016teawwaNoch keine Bewertungen
- Lexicon of Pharmacy: A Concise up-to-date referenceVon EverandLexicon of Pharmacy: A Concise up-to-date referenceNoch keine Bewertungen
- Documenting Clinical Interventions in Community Pharmacy PROMISe III Final ReportDokument74 SeitenDocumenting Clinical Interventions in Community Pharmacy PROMISe III Final ReportAbdul RehmanNoch keine Bewertungen
- Clinical Pharmacy PHR 405: Chapter 1: General ConsiderationsDokument24 SeitenClinical Pharmacy PHR 405: Chapter 1: General ConsiderationsSamiul Alam Rajib100% (1)
- Antimicrobial Guidelines 2012-13 PDFDokument84 SeitenAntimicrobial Guidelines 2012-13 PDFnydushNoch keine Bewertungen
- Home About This Website About The Exam News Syllabus Past Paper Saqs by Specialty Useful LinksDokument1 SeiteHome About This Website About The Exam News Syllabus Past Paper Saqs by Specialty Useful LinkskushishaNoch keine Bewertungen
- Drug Utilization ReviewsDokument7 SeitenDrug Utilization ReviewsenoyNoch keine Bewertungen
- Therapeutic Hypothermia - Principles, Indications, Practical ApplicationVon EverandTherapeutic Hypothermia - Principles, Indications, Practical ApplicationNoch keine Bewertungen
- Roles of Oncology Pharmacists in Korea 20140928Dokument17 SeitenRoles of Oncology Pharmacists in Korea 20140928adeputra25Noch keine Bewertungen
- Pharmacy: Undergraduate Study 2016Dokument18 SeitenPharmacy: Undergraduate Study 2016kgiyerNoch keine Bewertungen
- Research Design, Biostatistics, and Literature Evaluation: Ishaq Lat, Pharm.D., FCCP, FCCM, BCPSDokument18 SeitenResearch Design, Biostatistics, and Literature Evaluation: Ishaq Lat, Pharm.D., FCCP, FCCM, BCPSJeremy HamptonNoch keine Bewertungen
- Summer Training Handbook 2016Dokument48 SeitenSummer Training Handbook 2016Pooja Semwal BuganaNoch keine Bewertungen
- Drug Information Bulletin 52 05Dokument8 SeitenDrug Information Bulletin 52 05amritaryaaligarghNoch keine Bewertungen
- Biostatistics - CP For Pharm D IVDokument7 SeitenBiostatistics - CP For Pharm D IVjenisha ksNoch keine Bewertungen
- Contemporary Research Methods in Pharmacy and Health ServicesVon EverandContemporary Research Methods in Pharmacy and Health ServicesNoch keine Bewertungen
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingVon EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNoch keine Bewertungen
- Caprini DVT Risk AssessmentDokument2 SeitenCaprini DVT Risk AssessmentAnonymous PjQxbsJQaNoch keine Bewertungen
- 2 Design of DOSAGE DESIGNDokument16 Seiten2 Design of DOSAGE DESIGNMarjo100% (1)
- A Quick Reference For Managing Buprenorphine in The Perioperative SettingDokument3 SeitenA Quick Reference For Managing Buprenorphine in The Perioperative SettingJackie100% (1)
- Practice Standards, Training, and Professional Development: Curtis Haas, Pharm.D., FCCP, BCPSDokument34 SeitenPractice Standards, Training, and Professional Development: Curtis Haas, Pharm.D., FCCP, BCPSJeremy HamptonNoch keine Bewertungen
- 0 +Crtical+Care+Board+2022+Dokument948 Seiten0 +Crtical+Care+Board+2022+Amira HelayelNoch keine Bewertungen
- Prescription Medicines: A Practical GuideVon EverandPrescription Medicines: A Practical GuideBewertung: 2 von 5 Sternen2/5 (1)
- Critical Care Notes Clinical Pocket Guide - (Front Matter)Dokument10 SeitenCritical Care Notes Clinical Pocket Guide - (Front Matter)Britanny Nelson100% (1)
- Careers in Pharmacy PDFDokument32 SeitenCareers in Pharmacy PDFWalid WalidNoch keine Bewertungen
- Guidelines Emergency Medicine Pharmacist ServicesDokument15 SeitenGuidelines Emergency Medicine Pharmacist ServicesMárcio BatistaNoch keine Bewertungen
- Drug Information Bulletin 05 07Dokument4 SeitenDrug Information Bulletin 05 07amritaryaaligarghNoch keine Bewertungen
- UntitledDokument301 SeitenUntitledS.R.GNoch keine Bewertungen
- Adverse Reaction To DrugsDokument22 SeitenAdverse Reaction To DrugssridharNoch keine Bewertungen
- A Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsVon EverandA Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsBewertung: 3.5 von 5 Sternen3.5/5 (3)
- Familia y Terapia FamiliarDokument391 SeitenFamilia y Terapia FamiliarJesus Garcia AgamaNoch keine Bewertungen
- Textbook of Urgent Care Management: Chapter 34, Engaging Accountable Care Organizations in Urgent Care CentersVon EverandTextbook of Urgent Care Management: Chapter 34, Engaging Accountable Care Organizations in Urgent Care CentersNoch keine Bewertungen
- ABDokument8 SeitenABJia Weng FungNoch keine Bewertungen
- Microsoft Access 2016 Tutorial and Lab Manual: David MurrayDokument122 SeitenMicrosoft Access 2016 Tutorial and Lab Manual: David MurrayGizachewNoch keine Bewertungen
- Bps Psychiatric PharmacyDokument16 SeitenBps Psychiatric PharmacyMuhammad ZaitounNoch keine Bewertungen
- 201060antibiotics and ChildrenDokument2 Seiten201060antibiotics and ChildrencillenujmwNoch keine Bewertungen
- AAFP NyeriDokument40 SeitenAAFP Nyeriscan resepNoch keine Bewertungen
- The Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalDokument11 SeitenThe Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalBaru Chandrasekhar RaoNoch keine Bewertungen
- 3rd GenerationDokument3 Seiten3rd GenerationlorrainebarandonNoch keine Bewertungen
- PNLE Sample Questions NP2 NP5 & Drugs PDFDokument11 SeitenPNLE Sample Questions NP2 NP5 & Drugs PDFeric100% (1)
- PeritonitisDokument6 SeitenPeritonitisDiane ArgoteNoch keine Bewertungen
- Fracture ReportDokument19 SeitenFracture Reporteros_mimiNoch keine Bewertungen
- Bender Visual Motor Gestalt TestDokument39 SeitenBender Visual Motor Gestalt TestKent100% (1)
- Pereneal CareDokument2 SeitenPereneal CareindumathiNoch keine Bewertungen
- FMC Network Provider List - Dhaen2 Plan: Area Providers Name Provide RS Emirate SDokument39 SeitenFMC Network Provider List - Dhaen2 Plan: Area Providers Name Provide RS Emirate SMuhammad SiddiuqiNoch keine Bewertungen
- Annotated BibDokument8 SeitenAnnotated Bibapi-273086642Noch keine Bewertungen
- Good Clinical Practice PDFDokument4 SeitenGood Clinical Practice PDFdamera_vineetNoch keine Bewertungen
- Aims of The Subjective AssessmentDokument2 SeitenAims of The Subjective AssessmentAnonymous PQ4NOe2Noch keine Bewertungen
- The Role of The CRCDokument8 SeitenThe Role of The CRCSreeraj Guruvayoor SNoch keine Bewertungen
- GustationDokument1 SeiteGustationOlasunmbo Owolabi Afolayan100% (1)
- Zone Reiki Level 1Dokument14 SeitenZone Reiki Level 1Tineke100% (9)
- Development - of - CVS-5Dokument20 SeitenDevelopment - of - CVS-5Ahsan IslamNoch keine Bewertungen
- Antifungal DrugsDokument28 SeitenAntifungal DrugsKhairunnisa RasyidinNoch keine Bewertungen
- Health Emergency Kits Training 2019 PDFDokument33 SeitenHealth Emergency Kits Training 2019 PDFrema_rhere95Noch keine Bewertungen
- BÀI TẬP VỀ ĐỌC HIỂUDokument7 SeitenBÀI TẬP VỀ ĐỌC HIỂUNguyễn Việt HảiNoch keine Bewertungen
- Promotion MCQDokument17 SeitenPromotion MCQssamaddNoch keine Bewertungen
- Acute PainDokument3 SeitenAcute PainGerardeanne ReposarNoch keine Bewertungen
- Facilitator's Manual 2020 July 2020 FinalDokument176 SeitenFacilitator's Manual 2020 July 2020 Finalkaseera musaNoch keine Bewertungen
- Post AppliedDokument4 SeitenPost AppliedSumit EdwardNoch keine Bewertungen
- Genital HerpesDokument2 SeitenGenital HerpesWisnu WardanaNoch keine Bewertungen
- Umuagu Nnu DataDokument60 SeitenUmuagu Nnu DataJemilehin AbiodunNoch keine Bewertungen
- Friesen C4ST Amended Input HC Safety Code 6 - 140 Omitted Studies 224pDokument224 SeitenFriesen C4ST Amended Input HC Safety Code 6 - 140 Omitted Studies 224pSeth BarrettNoch keine Bewertungen
- Push Up Fact SheetDokument1 SeitePush Up Fact SheetNor AmalinaNoch keine Bewertungen
- Nordic Questionnaire For Low Back PainDokument5 SeitenNordic Questionnaire For Low Back Painbubbly_bea83% (6)
- Manual de Fixação Interna Rigida Craniofacial PDFDokument14 SeitenManual de Fixação Interna Rigida Craniofacial PDFFernandaJolyMacedoNoch keine Bewertungen
- Case of A Patient Having Congestive Heart FailureDokument13 SeitenCase of A Patient Having Congestive Heart Failuresykie joy albina100% (1)
- How To Make Ginger CandyDokument4 SeitenHow To Make Ginger CandyJun Jihad BarrogaNoch keine Bewertungen