Beruflich Dokumente
Kultur Dokumente
Pulmonary Hypertension and Various Treatment Options: Presented By: Cory Johanboeke
Hochgeladen von
Marie Petalcorin0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
8 Ansichten16 SeitenPPT
Originaltitel
Johan Bo Eke
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenPPT
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
8 Ansichten16 SeitenPulmonary Hypertension and Various Treatment Options: Presented By: Cory Johanboeke
Hochgeladen von
Marie PetalcorinPPT
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 16
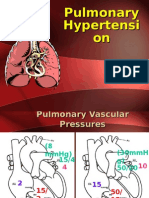
Pulmonary Hypertension
and Various Treatment
Options
Presented by: Cory
Johanboeke
Overview
Pulmonary hypertension is
characterized by increased pulmonary
arterial pressure and secondary right
ventricular failure.
PH is defined as a mean pulmonary
artery pressure greater 25mmHg at
rest or 30mmHg with exercise.
Classified into 5 groups according to
the mechanistic basis of the disease.
Classification
Group I Pulmonary arterial hypertension
(PAH), this group includes those with sporadic
idiopathic pulmonary arterial hypertension,
PAH due to collagen vascular disease (RA,
SLE, scleroderma), congenital heart defects
causing systemic to pulmonary shunt (ASD,
VSD), portal hypertension.
Pulmonary vascular resistance (PVR)
>120dynes/sec/cm, Pulmonary capillary
wedge pressure (PCWP)<15
Classification
Group II pulmonary venous
hypertension, which is pulmonary
hypertension due to left atrial,
ventricular, or valvular heart disease.
Group III - pulmonary hypertension is due
to disorders of the respiratory system or
hypoxemia (COPD, sleep apnea).
Group IV pulmonary hypertension is due
to chronic thrombotic or embolic disease
of the pulmonary vasculature
Classification
Group V pulmonary hypertension
due to inflammation, mechanical
obstruction, or extrinsic compression
of the pulmonary vasculature
( sarcoidosis, and fibrosing
mediastinitis)
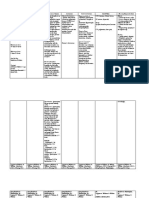
Pathophysiology
Increased blood flow in
the pulmonary
circulation
Hypoxic
vasoconstriction
Vascular fibrosis
Inflammatory mediators
causing vasoconstriction and
activating platelets
Smooth muscle cell
propagation
Increased vasculature
pressure
Right heart hypertrophy and
failure
Diagnostic test
Chest X-ray- enlargement of the central
pulmonary arteries, enlargement of the
right ventricle
EKG- signs of right atrial and ventricular
hypertrophy, right axis deviation
Echocardiography- used to estimate
pulmonary artery systolic pressure, and
right ventricle size and thickness, check for
shunts, valve function, and pericardial
effusions.
Diagnostic test
Pulmonary function test- to determine lung
disease as a cause.
Overnight oximetry- check for obstructive
sleep apnea
V/Q scan- check for thromboembolic disease.
Six minute walk to evaluate which NYHA
functional class the patient is in.
Right heart catheterization to confirm
diagnosis
Treatment options
primary therapy
Divided into two groups primary
therapy and advanced therapy.
Primary therapy is directed at
resolving the underlying cause.
Fix the underlying heart defect for
those in group 2
Diagnosis and treat the underlying
lung condition for those in group 3
Treatment options
primary therapy
Anticoagulation with warfarin for those in
class 4 (consider using with all classes) INR
goal of 2
Reversal of or treatment of underlying cause
in group 5
Use diuretics for peripheral edema and
hepatic congestion.
Oxygen 1-4 liters to maintain Sats. of 90% or
higher.
Exercise to improve functional capacity
Treatment options
advanced therapy
Indicated for all patients in New York Heart
Association (NYHA) functional class levels
3 or 4 (usually those with IPAH).
CCBs, Nifedipine and diltiazem, titrated up
to reduce patient to functional class 1 or 2
Prostonoid drugs, induce smooth muscle
relaxation and inhibit smooth muscle cell
and platelet aggregation. IV Epoprostenol,
SQ Treprostinil, inhaled Iloprost
Advanced therapy
Bosentan- Non-selective endothelin
receptor blocker (endothelin potent
vasoconstrictor)
Sixtaxentan, ambrisentan- selective
endothelin type A antagonist ( wont
block the vasodilator effects
mediated by type b receptors).
These drugs still under review by FDA
Advanced treatment
Sildenafil- phosphodiesterase type 5
inhibitor, prolongs the vasodilator effects of
Nitric oxide.
Milirone - phosphodiesterase type 3
inhibitor (vasodilator effect on both large
and small pulmonary arteries)
Nicorandil- potassium channel opener with
nitrate properties. (hyperpolarizes the
smooth muscle wall and calcium
antagonist).
Advanced therapy
Fasudil- approved to treat vasospasm
after arachnoid hemorrhage in Japan,
blocks Rho-kinase which is a
mediator of smooth muscle
contraction.
Surgical treatment options
Atrial septostomy- creates a right to left
shunt this increase systemic blood flow
and reduces pulmonary congestion.
Cadaveric lung transplantation
Living donor lobar lung transplantation-
harvesting lower lobes from healthy
donors and implanting them in the patient.
Das könnte Ihnen auch gefallen
- Cardiology NotesDokument13 SeitenCardiology NotesFreeNursingNotes78% (9)
- Portal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandPortal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Pulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHDokument59 SeitenPulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHbsaurabh20Noch keine Bewertungen
- Session 24 Heart FailureDokument15 SeitenSession 24 Heart Failuredreampurpose97Noch keine Bewertungen
- Heart Failure 1Dokument50 SeitenHeart Failure 1dhiraj parmar100% (1)
- Pulmonary Artery HypertensionDokument21 SeitenPulmonary Artery HypertensionAzizi Abd RahmanNoch keine Bewertungen
- Heartfailurepptsam 170511135108Dokument48 SeitenHeartfailurepptsam 170511135108enam professorNoch keine Bewertungen
- Heart FailureDokument28 SeitenHeart FailureStella CooKeyNoch keine Bewertungen
- Cme HFDokument30 SeitenCme HFTze SiangNoch keine Bewertungen
- Early Post-Operative Pulmonary Hypertension Management in The ICUDokument34 SeitenEarly Post-Operative Pulmonary Hypertension Management in The ICUari wijayantiNoch keine Bewertungen
- Pedal EdemaDokument45 SeitenPedal Edemafirdaushassan2112Noch keine Bewertungen
- Myocardial Infarction: Maj Aswathy Ganesh I Year MSC (N) Con, AfmcDokument45 SeitenMyocardial Infarction: Maj Aswathy Ganesh I Year MSC (N) Con, AfmcAswathy ganeshNoch keine Bewertungen
- Cardiac FailureDokument63 SeitenCardiac FailureNina OaipNoch keine Bewertungen
- Pulmonary HypertensionDokument4 SeitenPulmonary HypertensionFaisol Mong Ryong RizekiNoch keine Bewertungen
- Nursing Board Review CardioDokument16 SeitenNursing Board Review CardioPhilip Simangan100% (1)
- Surgical Critical Care ReviewDokument70 SeitenSurgical Critical Care ReviewSteven GodelmanNoch keine Bewertungen
- Left Ventricular FailureDokument17 SeitenLeft Ventricular Failurenisha24100% (1)
- СердечнаяDokument70 SeitenСердечнаяDaniel FunkNoch keine Bewertungen
- Approach To Patients With Possible Cardiovascular Disease and Physical Examination of The Cardiovascular SystemDokument79 SeitenApproach To Patients With Possible Cardiovascular Disease and Physical Examination of The Cardiovascular SystemLajel S. LachicaNoch keine Bewertungen
- 02.emergency CardiologyDokument135 Seiten02.emergency Cardiologyapi-19916399Noch keine Bewertungen
- Pulmonary HypertensionDokument54 SeitenPulmonary HypertensionmendaimashokombaNoch keine Bewertungen
- Acute HF-IAIDokument49 SeitenAcute HF-IAIAndita ListyannisaNoch keine Bewertungen
- Pharmacologic Agents in Heart Failure: Ayman Khdair, Ph.D. Wayne State University, Michigan, USADokument41 SeitenPharmacologic Agents in Heart Failure: Ayman Khdair, Ph.D. Wayne State University, Michigan, USAJalil HaddadinNoch keine Bewertungen
- Heart Failure: Classification, Risk Factors and Clinical FeaturesDokument48 SeitenHeart Failure: Classification, Risk Factors and Clinical FeaturesMaria Cristina Sierralta SimonNoch keine Bewertungen
- CH 46 Complications of AnaesthesiaDokument29 SeitenCH 46 Complications of AnaesthesiaChristian LeepoNoch keine Bewertungen
- Systolic Heart FailureDokument66 SeitenSystolic Heart FailureFerinaTarizaIINoch keine Bewertungen
- Heart FailureDokument44 SeitenHeart FailureSalman Habeeb100% (6)
- Aan 204 Group Coursework: in Partial Fulfillment of The Requirements For The CourseDokument118 SeitenAan 204 Group Coursework: in Partial Fulfillment of The Requirements For The CourseLucian CaelumNoch keine Bewertungen
- Pulm HTNDokument62 SeitenPulm HTNJonathan LongNoch keine Bewertungen
- Heart Failure Pelatihan Dokter KeluargaDokument55 SeitenHeart Failure Pelatihan Dokter KeluargaDelia NingrumNoch keine Bewertungen
- MF3 - Ischemic Heart DiseaseDokument28 SeitenMF3 - Ischemic Heart DiseaseAnnbe BarteNoch keine Bewertungen
- Cardiogenic ShockDokument49 SeitenCardiogenic Shockmaibejose0% (1)
- Lecture2 3Dokument44 SeitenLecture2 3Amanda HizerNoch keine Bewertungen
- Cardio Genic and Obstructive ShockDokument66 SeitenCardio Genic and Obstructive ShockdrkurniatiNoch keine Bewertungen
- Case Presentation: Congenital Heart DiseaseDokument37 SeitenCase Presentation: Congenital Heart DiseaseKarin Nadia UtamiNoch keine Bewertungen
- Heart Failure: Zelalem T., MD Yr III Resident, PediatricsDokument65 SeitenHeart Failure: Zelalem T., MD Yr III Resident, PediatricsChalie MequanentNoch keine Bewertungen
- Patofisiologi Shock CardiogenicDokument44 SeitenPatofisiologi Shock CardiogenicGalih Arief Harimurti Wawolumaja100% (1)
- Kuliah Pakar HF FKUMMDokument46 SeitenKuliah Pakar HF FKUMMOkta Dwi Kusuma AyuNoch keine Bewertungen
- Cardiovascular System: AnatomyDokument19 SeitenCardiovascular System: AnatomyStephanie MacVeighNoch keine Bewertungen
- Care of Patient With Pulmonary EmbolismDokument19 SeitenCare of Patient With Pulmonary Embolismtankmp100% (1)
- Kardiogenik SyokDokument43 SeitenKardiogenik SyokGalih Arief Harimurti WawolumajaNoch keine Bewertungen
- Cardiac Tamponade (Suryani)Dokument72 SeitenCardiac Tamponade (Suryani)Hamdani UsmanNoch keine Bewertungen
- Basics of AnesthesiaDokument34 SeitenBasics of Anesthesianicolinna2000yahoo.comNoch keine Bewertungen
- Cardiovascular Drugs: Dr. April Dawn R. LuceroDokument122 SeitenCardiovascular Drugs: Dr. April Dawn R. LuceroRjDNoch keine Bewertungen
- Respiratory Failure Results From Inadequate Gas ExchangeDokument7 SeitenRespiratory Failure Results From Inadequate Gas ExchangeJiezl Abellano AfinidadNoch keine Bewertungen
- Pharmacotherapy - Heart Failure - Dr. Mohammed KamalDokument62 SeitenPharmacotherapy - Heart Failure - Dr. Mohammed KamalMohammed KamalNoch keine Bewertungen
- Vasopressors and Inotropes in ShockDokument8 SeitenVasopressors and Inotropes in ShockRiska PashaNoch keine Bewertungen
- SEMINARDokument31 SeitenSEMINARDeveshNoch keine Bewertungen
- Hypertension For EMS ProvidersDokument35 SeitenHypertension For EMS ProvidersPaulhotvw67100% (5)
- HTA Eng NouaDokument56 SeitenHTA Eng NouaAnna HaritonencoNoch keine Bewertungen
- Cardiac Content WyattDokument90 SeitenCardiac Content WyattAnni BarbaNoch keine Bewertungen
- 5 Shock PPT EnglishDokument77 Seiten5 Shock PPT EnglishKessi VikaneswariNoch keine Bewertungen
- Congestive Cardiac FailureDokument49 SeitenCongestive Cardiac FailureHampson MalekanoNoch keine Bewertungen
- SHOCKDokument17 SeitenSHOCKChithra Saju100% (1)
- Clinical Case - 1Dokument51 SeitenClinical Case - 1Moush AbdiNoch keine Bewertungen
- Dilated Cardiomyopathy: DR Adekunle Victor O. Cardiology Unit Medicine Department Abuth Shika ZariaDokument26 SeitenDilated Cardiomyopathy: DR Adekunle Victor O. Cardiology Unit Medicine Department Abuth Shika ZariaVictor AdekunleNoch keine Bewertungen
- Atrial Fibrillation (AF)Dokument24 SeitenAtrial Fibrillation (AF)farmasi_hm100% (1)
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Dokument81 SeitenHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNoch keine Bewertungen
- Preoperative Assessment - Doctor'sDokument15 SeitenPreoperative Assessment - Doctor'sbz6dgr4gsvNoch keine Bewertungen
- How The Body Converts Food To Energy: K. DunlapDokument65 SeitenHow The Body Converts Food To Energy: K. DunlapMarie PetalcorinNoch keine Bewertungen
- DifferentialDokument2 SeitenDifferentialMarie PetalcorinNoch keine Bewertungen
- Management of Bacterial MeningitisDokument11 SeitenManagement of Bacterial MeningitisMarie PetalcorinNoch keine Bewertungen
- SeizuresDokument3 SeitenSeizuresMarie PetalcorinNoch keine Bewertungen
- Connective TissueDokument2 SeitenConnective TissueMarie PetalcorinNoch keine Bewertungen
- Trematodes 2Dokument4 SeitenTrematodes 2Marie Petalcorin100% (1)
- Pefr and Fet: Cabaron, Mary Gwen Frosi Petalcorin, Marie FrauleinDokument8 SeitenPefr and Fet: Cabaron, Mary Gwen Frosi Petalcorin, Marie FrauleinMarie PetalcorinNoch keine Bewertungen
- High Frequency VentilationDokument33 SeitenHigh Frequency VentilationMarie PetalcorinNoch keine Bewertungen
- Instrumental Analysis: Spectrophotometric MethodsDokument32 SeitenInstrumental Analysis: Spectrophotometric MethodsMarie PetalcorinNoch keine Bewertungen
- Is Lab Cheat Sheet FINALDokument9 SeitenIs Lab Cheat Sheet FINALMarie PetalcorinNoch keine Bewertungen
- Transport of Oxygen and Carbon Dioxide-PartialDokument24 SeitenTransport of Oxygen and Carbon Dioxide-PartialMarie PetalcorinNoch keine Bewertungen
- High Frequency VentilationDokument33 SeitenHigh Frequency VentilationMarie PetalcorinNoch keine Bewertungen
- Beyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFDokument56 SeitenBeyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFMarie Petalcorin100% (1)
- Beyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFDokument56 SeitenBeyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFMarie Petalcorin100% (1)
- Tamil Nadu Treatment Guidelines PDFDokument8 SeitenTamil Nadu Treatment Guidelines PDFsekarchand33Noch keine Bewertungen
- Synthesis of Procaine PDFDokument3 SeitenSynthesis of Procaine PDFLive FlightsNoch keine Bewertungen
- CompoundingDokument36 SeitenCompoundingSarah :-)Noch keine Bewertungen
- EORTC Guidelines 2017Dokument18 SeitenEORTC Guidelines 2017Cata RodriguezNoch keine Bewertungen
- Prescription - 5540767 - 08 02 2023 - Undefined - Apollo 2471677073378588Dokument2 SeitenPrescription - 5540767 - 08 02 2023 - Undefined - Apollo 2471677073378588Nirav ShahNoch keine Bewertungen
- Physiology of Pain in LabourDokument29 SeitenPhysiology of Pain in LabourRed Williams50% (2)
- Otc GITDokument142 SeitenOtc GITMai MosaadNoch keine Bewertungen
- Levin 2002Dokument18 SeitenLevin 2002Gabriel FidelisNoch keine Bewertungen
- CV Brown 04232021Dokument9 SeitenCV Brown 04232021api-536548646Noch keine Bewertungen
- SchizophreniaDokument26 SeitenSchizophreniapranesh premkumarNoch keine Bewertungen
- Topic 2 - Biologically - Based Therapy Learning Objectives:: ExploreDokument6 SeitenTopic 2 - Biologically - Based Therapy Learning Objectives:: ExploreHope JouleNoch keine Bewertungen
- Lecture-4.Drug Metabolism and EliminationDokument47 SeitenLecture-4.Drug Metabolism and EliminationC/fataax C/xakiimNoch keine Bewertungen
- IbandronateDokument2 SeitenIbandronatePratik R JobaliaNoch keine Bewertungen
- Cannabis Toxic EffectsDokument9 SeitenCannabis Toxic EffectsOsvaldo CortésNoch keine Bewertungen
- Final Salbu-IpraDokument3 SeitenFinal Salbu-IpraGwyn RosalesNoch keine Bewertungen
- Experience Limits For First Year Speciaty Training 2019 (The Savvy IMG)Dokument1 SeiteExperience Limits For First Year Speciaty Training 2019 (The Savvy IMG)SaurabhNoch keine Bewertungen
- Knoll Price ListDokument16 SeitenKnoll Price ListkadapanehruparkyogaNoch keine Bewertungen
- MK Notes by YournursingspaceDokument60 SeitenMK Notes by Yournursingspaceezinne obinna-umaNoch keine Bewertungen
- Nitrosamine Contamination in Pharmaceuticals - Threat, Impact, and ControlDokument11 SeitenNitrosamine Contamination in Pharmaceuticals - Threat, Impact, and ControlliêmNoch keine Bewertungen
- Leflunomide in DogsDokument6 SeitenLeflunomide in DogsLuluu CortésNoch keine Bewertungen
- VSim Pharm (Mary Richards)Dokument3 SeitenVSim Pharm (Mary Richards)Jay Blastic's arts and FunNoch keine Bewertungen
- Notes - Lec 20 - Antimycobacterial AgentsDokument14 SeitenNotes - Lec 20 - Antimycobacterial AgentsChesmar MacapalaNoch keine Bewertungen
- Peripheral Nervous System (PNS) : 1. Anatomical ClassificationDokument4 SeitenPeripheral Nervous System (PNS) : 1. Anatomical ClassificationShafiq ZahariNoch keine Bewertungen
- Treatment and Management of Mental Health Conditions During Pregnancy and Postpartum ACOG June 2023Dokument27 SeitenTreatment and Management of Mental Health Conditions During Pregnancy and Postpartum ACOG June 2023kaiorm2k100% (3)
- KEM Protocols - Hypertensive Emergency (Dr. Pritha)Dokument3 SeitenKEM Protocols - Hypertensive Emergency (Dr. Pritha)Sonu AntonyNoch keine Bewertungen
- Anticholinergic Drugs11Dokument12 SeitenAnticholinergic Drugs11Deep kumarNoch keine Bewertungen
- Biocompatibility Test Methods - Pacific BioLabsDokument11 SeitenBiocompatibility Test Methods - Pacific BioLabsAnil KumarNoch keine Bewertungen
- Managed Entry AgreementsDokument21 SeitenManaged Entry AgreementsRenato Nogueira dos SantosNoch keine Bewertungen
- Drug Study - Ibs - Sanguyo, C.BDokument15 SeitenDrug Study - Ibs - Sanguyo, C.BCamille SanguyoNoch keine Bewertungen
- Mat Presentation 1Dokument23 SeitenMat Presentation 1api-649066372Noch keine Bewertungen