Beruflich Dokumente
Kultur Dokumente
One Lung Ventilation: Llalando L. Austin Ii, MHSC, Aa-C, RRT Nova Southeastern University
Hochgeladen von
ZulkarnainBustamam100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
69 Ansichten47 Seitenone lung ventilation
Originaltitel
One Lung Ventilation 1
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenone lung ventilation
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
69 Ansichten47 SeitenOne Lung Ventilation: Llalando L. Austin Ii, MHSC, Aa-C, RRT Nova Southeastern University
Hochgeladen von
ZulkarnainBustamamone lung ventilation
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 47
One Lung Ventilation
Llalando L. Austin II, MHSc,
AA-C, RRT
Nova Southeastern University
Objectives
Describe One Lung Ventilation
Understand the methods for securing one lung
ventilation
Learn the indications and contraindications for
each procedure
Understand hypoxic pulmonary vasoconstriction
(HPV)
Understand commonly associated surgical
procedures that require one lung ventilation
Common techniques and supplies for one lung
ventilation
Understand the case setup and patient
preparation for the procedure
Thoracotomy
Thoracotomy with Lung
Deflated
VATS
VATS
VATS
What is One Lung Ventilation
(OLV)?
It is the intentional collapse of a lung on
the operative side of the patient which
facilitates most thoracic procedures.
Requires much skill of the anesthesia
team
Difficult to place lung isolation equipment
Ability to overcome hypoxic pulmonary
vasoconstriction
Patient population is comparably sicker
Definition of Terms
Dependent Lung or Down Lung
The lung that is ventilated
Non-dependent Lung or Up Lung
The lung that is collapsed to facilitate
the surgery
Methods of Lung Separation
Bronchial blockers
Single-lumen tracheal tubes w/ a bronchial blocker
(Univent)
Arterial embolectomy catheter (ie Fogarty)
Single-lumen endobronchial tubes
Gordon-Green tube (carinal hook)
Double-lumen endobronchial tubes
Robert-Shaw (R or L), Carlens (R), White (L)
Carlens and White both have carinal hooks
From 35Fr to 41Fr (35, 37, 39, 41)
26Fr smallest size
Used for children as young as 8 years
28Fr and 32Fr used for pediatric patients 10 and older
Double Lumen Tubes
Patient Monitoring
Considerations
Direct arterial catheterization (a-line)
essential for nearly all thoracic cases
Allows for beat-to-beat blood pressure analysis
Sampling for determination of ABG
Central venous pressure monitoring (central line)
essential for measuring right atrial and right ventricular
pressures
Useful in monitoring:
large volume shifts
hypovolemia
need for vasoactive drugs
Pulmonary artery catheterization
left sided filling pressures, cardiac output
Calculation of derived hemodynamic and respiratory
parameters and clinical use of Starling curve
Most PA catheters (more than 90%) float to and locate in the
right lung due to increased pulmonary blood flow
Create inaccurate reading for R thoracotomies
Patient Monitoring
Considerations
Oxygenation and Ventilation
Monitoring inspired oxygen
Sampling of arterial blood for ABGs
Pulse oximetry
Transcutaneous oxygen tension
for neonates
Qualitative signs
chest expansion
observation of reservoir bag
auscultation of breath sounds
EtCO2 measurement, capnograph
Indications for One-Lung
Ventilation
Absolute
Isolation of one lung from another to
prevent spillage or contamination
(infection, massive hemorrhage)
Control of distribution of ventilation
Bronchopleural fistula
Surgical opening of major conducting airway
Unilateral bronchopulmonary lavage
Ex: pulmonary alveolar proteinosis
Indications for One-Lung
Ventilation
Relative
Surgical exposure- high priority
Thoracic aortic aneurysm
Pneumonectomy
Upper lobectomy
Surgical exposure- lower priority
Middle lobe lobectomies
Esophageal resection
Thoracoscopy
Thoracic spine procedures
Post-removal of totally-occluding chronic
unilateral pulmonary emboli
Double Lumen Endobronchial
Tubes
Double Lumen Endobronchial
Tubes
Advantages
Relatively easy to place
Allow conversion back and forth from OLV to
two-lung ventilation
Allow suctioning of both lungs individually
Allow CPAP to be applied to the non-
dependent lung
Allow PEEP to be applied to the dependent
lung
Ability to ventilate around scope in the tube
Disadvantages
Cannot take patient to PACU or the
Unit
Must be changed out for a regular
ETT if post-op ventilation
Correct positioning is dependent on
appropriate size for height of patient
Length of trachea
DLT Placement
Prepare and check tube
Ensure cuff inflates and deflates
Lubricate tube
Insert tube with distal concave curvature facing
anteriorly
Remove stylet once through the vocal cords
Rotate tube 90 degrees (in direction of desired
lung)
Advancement of tube ceases when resistance is
encountered. Average lip line is 29 2 cm.
*If a carinal hook is present, must watch hook go
through cords to avoid trauma to them.
DLT Placement
Check for placement by auscultation
Inflate tracheal cuff- expect equal lung ventilation
Clamp the white side (marked "tracheal" for left-sided tube)
and remove cap from the connector
Expect some left sided ventilation through bronchial lumen,
and some air leak past bronchial cuff, which is not yet inflated
Slowly inflate bronchial cuff until minimal or no leak is
heard at uncapped right connector
Go slow- it only requires 1-3 cc of gas and bronchial rupture is
a risk
Remove the clamp and replace the cap on the tracheal side
Check that both lungs are ventilated
Selectively clamp each side, and expect visible chest
movement and audible breath sounds only on the right
when left is clamped, and vice versa
DLT Placement
Checking tube placement with the fiberoptic
bronchoscope
Several situations exist where auscultation maneuvers are
impossible (patient is prepped and draped), or when they
do not provide reliable information (preexisting lung disease
so that breath sounds are not very audible, or if the tube is
only slightly malpositioned)
The double-lumen tube's precise position can be most
reliably determined with the fiberoptic bronchoscope
In patients with double-lumen tubes whose position seemed
appropriate to auscultations, 48% had some degree of
malposition. So always check position with fiberoptic
After advancing the fiberoptic scope thru the tracheal
tube you should see the bronchial blue balloon in a semi
lunar shape, just peeking out of the bronchus
DLT Placement
Wire-Guided Endobronchial
Blockers
Advantages
Quickly and precisely navigate the airway
The guide wire loop couples the pediatric fiberoptic
bronchoscope and the wire-guided endobronchial blocker
yet both remain able to move independently of each other and
the pediatric fiberoptic bronchoscope may navigate the airway
independent of its role in carrying the endobronchial blocker
The pediatric bronchoscope acts as a guide, allowing the
endobronchial blocker to be advanced over it into the
correct position
In addition, the wire-guided endobronchial blocker allows
one-lung ventilation with a single-lumen endotracheal tube
Thus, one-lung ventilation is not dependent on installing a
special device in the airway, such as a double-lumen tube or a
Univent endotracheal tube
Allows one-lung ventilation in the critically ill patient in whom
reintubation may be difficult or impossible and in patients with
a known difficult airway requiring fiberoptic intubation with a
conventional endotracheal tube
Unnecessary to convert from a conventional double-lumen
endotracheal tube to a single-lumen tube at the end of surgery
Disadvantages
Satisfactory bronchial seal and lung separation are sometimes
difficult to achieve
The blocked lung collapses slowly (and sometimes
incompletely)
The balloon may become dislodged during surgery and enter
the trachea proper, causing a complete airway obstruction
In situations of acute increases in airway pressure, the
endobronchial blocker balloon should be immediately deflated and
the blocker re-advanced
It will then re-enter the correct segment (as the tip remains in the
correct bronchus and only the proximal balloon portion has entered
the trachea)
In this case, a pediatric fiberoptic bronchoscope should be re-
introduced into the airway and the balloon re-positioned
In order to prevent barotrauma, the initial balloon inflation volume
should not be exceeded
It is important that the balloon be fully deflated when not in use
and only be re-inflated with the same volume used during
positioning and bronchoscopy.
Indications for Wire-Guided
Endobronchial Blockers vs. DLT
Critically ill patients
Rapid sequence induction
Known and unknown difficult airway
Postoperative intubation
Small adult and pediatric patients
Obese adults
Wire-Guided Endobronchial
Blockers
Wire-Guided Endobronchial
Blockers
Wire-Guided Endobronchial
Blockers
Available sizes
Adult 9 Fr
Pediatric 5 Fr
Wire-Guided Endobronchial
Blockers
Wire-Guided Endobronchial
Blockers
Wire-Guided Endobronchial
Blockers
Wire-Guided Endobronchial
Blockers
Fogarty Embolectomy
Catheters
Fogarty Embolectomy
Catheter
Single-lumen balloon tipped catheter with a removable
stylet
In the parallel fashion, the Fogarty catheter is inserted
prior to intubation
In the co-axial fashion, the Fogarty catheter is placed
through the endotracheal tube
Both techniques require fiberoptic bronchoscopy to
direct the Fogarty catheter into the correct pulmonary
segment
Once the catheter is in place, the balloon is inflated,
sealing the airway
Clinical limitations to the Fogarty technique
Difficult to direct and cannot be coupled to a fiberoptic bronchoscope
No accessory lumen for either removal of gas from the blocked segment or
insufflation of oxygen to reverse hypoxemia
Ventilate w/ 100% O2 prior to balloon inflation to aid in gas removal
Univent Tubes
Univent Tubes
Endotracheal intubation can be performed in the conventional
manner, just like a single lumen endotracheal tube
One-lung ventilation can be achieved by placement of the blocker
to either the left or right lung, or to lung segments
Insufflation and CPAP can be achieved through the lumen of the
blocker shaft
Blocked lung can be collapsed by aspirating air through the lumen
of the blocker shaft
The blocker can be retracted into its pocket to facilitate post-
operative ventilation
Improved "torque control" bronchial blocker:
- Easier to direct by twisting than previous nylon catheter
- High torque control malleable shaft for smooth intubation
- Flexible blocker shaft with softer open lumen tip
- Latex-free
Comparison of Various Tube
Diameters
Complications of One Lung
Ventilation
All difficult airway complications
Injury to lips, mouth, teeth
Injury to airway mucosa from stylet
Bronchial Rupture
Decreased saturation
HPV
Inability to isolate lung
Complications - Bronchial
Rupture
Hypoxic Pulmonary
Vasoconstriction
Hypoxia is a powerful stimulus for
pulmonary vascular constriction
Bodys mechanism to divert blood flow
away from areas of no ventilation to areas
of ventilation
Vasoconstriction that decreases blood flow
from alveoli that are not ventilated to
alveoli that are ventilated
Bodys way to decrease the shunt that was
created by change
Position
V/Q mismatch
HPV
Bodys compensatory mechanism for
hypoxia
Clinical Notes:
Direct acting vasodilators inhibit HPV response
Volatile agents at higher concentrations inhibit
HPV response
No HPV =
Increases shunt
Decreases PaO2
Management of Hypoxia in One
Lung Ventilation
100% FIO2
10 mL/kg tidal volume
Do not change the tidal volume from 2 lung ventilation
Maintain normocapnia
Maintain correct tube position
Suction both lungs
Apply PEEP to dependant lung
Apply CPAP to non-dependant lung
Re-inflate collapsed lung at various intervals
Extreme cases
Clamp the pulmonary artery to collapsed lung
Case Setup for DLT & OLV
MSMAID
Preferred blade and handle
Airway Have standard supplies &
assortment of sizes for DLT or other OLV
choice equipment
Fiberoptic cart
Hemostats or clamps to clamp off lumens
of the tube
Suction!!
References
http://ourworld.cs.com/_ht_a/doschk/onelung.
htm
Finucane and Santora
Morgan and Mikhail
Barash, Cullen, Stoelting
Das könnte Ihnen auch gefallen
- Anesthesia Management in Bronchoscopy Procedure NewDokument29 SeitenAnesthesia Management in Bronchoscopy Procedure NewChlara Obisuru100% (1)
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideVon EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuideNoch keine Bewertungen
- Paediatric Anaesthesia PDFDokument33 SeitenPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriNoch keine Bewertungen
- Preanesthetic Medication JasminaDokument44 SeitenPreanesthetic Medication Jasminaanjali sNoch keine Bewertungen
- Prehospital Anesthesia HandbookDokument46 SeitenPrehospital Anesthesia HandbookoscarNoch keine Bewertungen
- Pediatric Anesthesia: A Guide for the Non-Pediatric Anesthesia ProviderVon EverandPediatric Anesthesia: A Guide for the Non-Pediatric Anesthesia ProviderNoch keine Bewertungen
- Anesthesia PresentationDokument19 SeitenAnesthesia PresentationJohnyNoch keine Bewertungen
- Graphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaVon EverandGraphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaNoch keine Bewertungen
- ERAS Guidelines PDFDokument8 SeitenERAS Guidelines PDFWadezigNoch keine Bewertungen
- 029 Reddy PDFDokument59 Seiten029 Reddy PDFKonas Xi PalembangNoch keine Bewertungen
- Neonatal ResuscitationDokument7 SeitenNeonatal ResuscitationJavier López García100% (1)
- Awareness Under AnesthesiaDokument27 SeitenAwareness Under AnesthesiaagatakassaNoch keine Bewertungen
- Anesthesia Resident Requirements PDFDokument21 SeitenAnesthesia Resident Requirements PDFJulieNoch keine Bewertungen
- Preoperative Patient Assessment and Management: Roxanne Jeen L. FornollesDokument61 SeitenPreoperative Patient Assessment and Management: Roxanne Jeen L. FornollesRyan FornollesNoch keine Bewertungen
- TIVA - Copy (2) - Copy-1Dokument34 SeitenTIVA - Copy (2) - Copy-1Keerthikumar Parvatha100% (2)
- Anesthetic Machine For StudentDokument76 SeitenAnesthetic Machine For StudentMohmmed MousaNoch keine Bewertungen
- REVIEW Anesthesia For Thoracic Surgery PDFDokument22 SeitenREVIEW Anesthesia For Thoracic Surgery PDFcristinaNoch keine Bewertungen
- Anesthesia For GeriatricDokument21 SeitenAnesthesia For GeriatricintanNoch keine Bewertungen
- Fred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008Dokument53 SeitenFred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008lmjeksoreNoch keine Bewertungen
- Safe Pediatric AnesthesiaDokument24 SeitenSafe Pediatric AnesthesiamdNoch keine Bewertungen
- Obstetrics AnesthesiaDokument31 SeitenObstetrics AnesthesiaNorfarhanah ZakariaNoch keine Bewertungen
- Management of Intraoperative Bronchospasm: Dr. ImranDokument49 SeitenManagement of Intraoperative Bronchospasm: Dr. ImranhellodrvigneshwarNoch keine Bewertungen
- Airway ManagementDokument48 SeitenAirway ManagementRea Dominique CabanillaNoch keine Bewertungen
- Local Anesthesia ToxicityDokument5 SeitenLocal Anesthesia ToxicityvelangniNoch keine Bewertungen
- Epidural Anatomy & PhysiologyDokument14 SeitenEpidural Anatomy & PhysiologyAbel AxelNoch keine Bewertungen
- Anesthesia ManualDokument21 SeitenAnesthesia ManualDocFrankNoch keine Bewertungen
- Technique For Awake Fibre Optic IntubationDokument3 SeitenTechnique For Awake Fibre Optic Intubationmonir61Noch keine Bewertungen
- Obestetrics GynecologyDokument203 SeitenObestetrics GynecologySwamynadh Gandhi ReddiNoch keine Bewertungen
- Bier Block (Intravenous Regional Anesthesia), Handout PDFDokument8 SeitenBier Block (Intravenous Regional Anesthesia), Handout PDFjahangirealamNoch keine Bewertungen
- Complications of Spinal and Epidural AnesthesiaDokument45 SeitenComplications of Spinal and Epidural AnesthesiashikhaNoch keine Bewertungen
- Failed Spinal Anesthesia PDFDokument2 SeitenFailed Spinal Anesthesia PDFShamim100% (1)
- Skeletalmusclerelaxants 151101095949 Lva1 App6891 PDFDokument69 SeitenSkeletalmusclerelaxants 151101095949 Lva1 App6891 PDFvvb_frndNoch keine Bewertungen
- Enhanced Recovery After Surgery: Nutrition Issues in Gastroenterology, Series #151Dokument15 SeitenEnhanced Recovery After Surgery: Nutrition Issues in Gastroenterology, Series #151Hendry DimasNoch keine Bewertungen
- Pa Sample QuestionsDokument1 SeitePa Sample QuestionsJokevin Prasetyadhi100% (1)
- Extubation After AnaesthesiaDokument7 SeitenExtubation After AnaesthesiaaksinuNoch keine Bewertungen
- Conduct of AnaesthesiaDokument30 SeitenConduct of AnaesthesiaAnirban PalNoch keine Bewertungen
- Anesthesia For Genitourinary SurgeryDokument76 SeitenAnesthesia For Genitourinary SurgeryWenny Eka FildayantiNoch keine Bewertungen
- Color Code Anesthesia PDFDokument6 SeitenColor Code Anesthesia PDFYusnia Gulfa MaharaniNoch keine Bewertungen
- Update EmergenciesDokument84 SeitenUpdate EmergenciesElaineNoch keine Bewertungen
- Awareness in Anesthesia FinalisedDokument42 SeitenAwareness in Anesthesia FinalisedLean CyNoch keine Bewertungen
- Comparison of Two Approaches ofDokument96 SeitenComparison of Two Approaches ofJacob OrtizNoch keine Bewertungen
- Airway ManagmentDokument42 SeitenAirway Managmentkader abdiNoch keine Bewertungen
- AA Course-Difficult Airway1Dokument54 SeitenAA Course-Difficult Airway1Anonymous V5xDcrNoch keine Bewertungen
- Anaesthetic Management of Joint Replacement SurgeriesDokument55 SeitenAnaesthetic Management of Joint Replacement SurgeriesRaguNoch keine Bewertungen
- Anaesthesia and Sedation Outside TheatresDokument15 SeitenAnaesthesia and Sedation Outside Theatresمحمد زينNoch keine Bewertungen
- Rapid Seq InductionDokument6 SeitenRapid Seq InductionandikszuhriNoch keine Bewertungen
- Checklist For Anaesthetic Equipment 2012Dokument2 SeitenChecklist For Anaesthetic Equipment 2012that dude in duettesNoch keine Bewertungen
- 04.06.2018 - 6 - V. Kushakovsky - Pediatric AnaesthesiaDokument46 Seiten04.06.2018 - 6 - V. Kushakovsky - Pediatric AnaesthesiaPhilippe KinnaerNoch keine Bewertungen
- Anesthesia For Orthopedic SurgeryDokument27 SeitenAnesthesia For Orthopedic Surgeryjeremy_raineyNoch keine Bewertungen
- Factors Affectin Block HeightDokument37 SeitenFactors Affectin Block HeightshikhaNoch keine Bewertungen
- Thoracic 53Dokument53 SeitenThoracic 53RaMy “MhMd” ElaRabyNoch keine Bewertungen
- General-Anesthesia Part 2Dokument6 SeitenGeneral-Anesthesia Part 2Dianne GalangNoch keine Bewertungen
- Bob Peripheral Nerve Blocks AspanDokument70 SeitenBob Peripheral Nerve Blocks AspanPrunaru BogdanNoch keine Bewertungen
- SRNA Orientation ChecklistDokument40 SeitenSRNA Orientation Checklistihtisham1Noch keine Bewertungen
- General AnestDokument35 SeitenGeneral AnestMauz AshrafNoch keine Bewertungen
- Anesthesia Machine CircuitsDokument41 SeitenAnesthesia Machine CircuitsDidi OkNoch keine Bewertungen
- Anaesthesia Equipment: Anaesthetics OSCE (Compiled by C Lee Kin) 1Dokument98 SeitenAnaesthesia Equipment: Anaesthetics OSCE (Compiled by C Lee Kin) 1Shen BNoch keine Bewertungen
- IV Induction Agents UMAIDDokument63 SeitenIV Induction Agents UMAIDUmaid Mirza100% (1)
- Analgesia New DrugsDokument40 SeitenAnalgesia New DrugsZulkarnainBustamamNoch keine Bewertungen
- Guillain-Barré SyndromeDokument21 SeitenGuillain-Barré SyndromeZulkarnainBustamamNoch keine Bewertungen
- CV Prof Husni TanraDokument1 SeiteCV Prof Husni TanraZulkarnainBustamamNoch keine Bewertungen
- Trauma Dan Sepsis 2Dokument16 SeitenTrauma Dan Sepsis 2ZulkarnainBustamamNoch keine Bewertungen
- DR Pauline Kane Registrar in Palliative Medicine Beaumont Hospital 17 Sept 2009Dokument40 SeitenDR Pauline Kane Registrar in Palliative Medicine Beaumont Hospital 17 Sept 2009ZulkarnainBustamamNoch keine Bewertungen
- Garuda Indonesia: Electronic Ticket ReceiptDokument2 SeitenGaruda Indonesia: Electronic Ticket ReceiptZulkarnainBustamamNoch keine Bewertungen
- @anesthesia Books 2013 Board StiffDokument302 Seiten@anesthesia Books 2013 Board StiffZulkarnainBustamamNoch keine Bewertungen
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDokument49 SeitenAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNoch keine Bewertungen
- Anionic GapDokument6 SeitenAnionic GapZulkarnainBustamamNoch keine Bewertungen
- Defination and Types of Anionic GapDokument6 SeitenDefination and Types of Anionic GapZulkarnainBustamamNoch keine Bewertungen
- Pain Management - Delhi.data - WsDokument23 SeitenPain Management - Delhi.data - WsZulkarnainBustamamNoch keine Bewertungen
- Fins'12 1 2Dokument125 SeitenFins'12 1 2Brutus AntonyNoch keine Bewertungen
- 66Dokument84 Seiten66Jimmy Jimmy0% (1)
- Blocked Fallopian Tubes and Its Management With AyDokument2 SeitenBlocked Fallopian Tubes and Its Management With AywinodhelloNoch keine Bewertungen
- ATLS Practice Test 3 Answers & ExplanationsDokument10 SeitenATLS Practice Test 3 Answers & ExplanationsCarl Sars50% (2)
- Ureteroscopy G AdeyDokument66 SeitenUreteroscopy G AdeyCentanarianNoch keine Bewertungen
- The Swing Lock Denture Its Use in Conventional Removable Partial Denture Prosthodontics PDFDokument3 SeitenThe Swing Lock Denture Its Use in Conventional Removable Partial Denture Prosthodontics PDFscott_c_kane100% (1)
- CASE STUDIES L3 A Group 2Dokument3 SeitenCASE STUDIES L3 A Group 2Abdul Hamid NoorNoch keine Bewertungen
- Operative Gyn MCQ PDFDokument10 SeitenOperative Gyn MCQ PDFFentahun TadesseNoch keine Bewertungen
- Chapter 7Dokument34 SeitenChapter 7Hima AlqahtaniNoch keine Bewertungen
- Penile Anomalies in AdolescenceDokument10 SeitenPenile Anomalies in AdolescenceIoannis ValioulisNoch keine Bewertungen
- 09 Catastrophe Cover 2011 5.1Dokument2 Seiten09 Catastrophe Cover 2011 5.1Tufha NiwaNoch keine Bewertungen
- Dr. Ahmed Fathalla IbrahimDokument21 SeitenDr. Ahmed Fathalla IbrahimHevin GokulNoch keine Bewertungen
- Gorean Treatments and ServesDokument3 SeitenGorean Treatments and ServesNishaNightFireNoch keine Bewertungen
- Dcia (Deep Circumflex Iliac Artery) FlapDokument43 SeitenDcia (Deep Circumflex Iliac Artery) FlapRohit SharmaNoch keine Bewertungen
- 9 9 2023Dokument10 Seiten9 9 2023hoangnam147680Noch keine Bewertungen
- Cardiomyopathy: Restrictive Heart DiseaseDokument18 SeitenCardiomyopathy: Restrictive Heart DiseaseMitch GabuyaNoch keine Bewertungen
- Chest TubeDokument8 SeitenChest TubetanabalrajNoch keine Bewertungen
- Eras Part 1Dokument15 SeitenEras Part 1erani sukmaNoch keine Bewertungen
- Nitrous Oxide Inhalation Is A Safe and Effective Way To Facilitate Procedures in Paediatric Outpatient DepartmentsDokument4 SeitenNitrous Oxide Inhalation Is A Safe and Effective Way To Facilitate Procedures in Paediatric Outpatient DepartmentsfebyNoch keine Bewertungen
- Cardiac PhysiologyDokument102 SeitenCardiac PhysiologyPeter Larsen100% (1)
- 70 Neonatal Anaesthesia 2 Anaesthesia For Neonates With Abdominal Wall DefectsDokument10 Seiten70 Neonatal Anaesthesia 2 Anaesthesia For Neonates With Abdominal Wall DefectsParvathy R NairNoch keine Bewertungen
- Kuwait Pediatric GuideLinesDokument124 SeitenKuwait Pediatric GuideLinesAlwaallh MohammedNoch keine Bewertungen
- Kewenangan Klinis SP - JPDokument3 SeitenKewenangan Klinis SP - JPVania Lystia TantraNoch keine Bewertungen
- Set Rec Pic 899Dokument12 SeitenSet Rec Pic 899Peter SalimNoch keine Bewertungen
- Incise Drape CatalogueDokument10 SeitenIncise Drape CatalogueShadreck MabvoroNoch keine Bewertungen
- Gastrectomy Case AnalysisDokument1 SeiteGastrectomy Case AnalysisJayAnnPaclipanNoch keine Bewertungen
- PeriopConceptsDokument43 SeitenPeriopConceptsKysha Huang100% (1)
- SURGERY Breast DiseasesDokument25 SeitenSURGERY Breast DiseasesBiplav SinghNoch keine Bewertungen
- Essentials of Anatomy and Physiology 5th Edition Scanlon ch01Dokument28 SeitenEssentials of Anatomy and Physiology 5th Edition Scanlon ch01ellieNoch keine Bewertungen
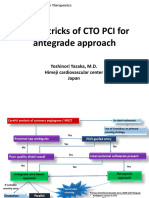
- Tips & Tricks of CTO PCI For Antegrade Approach: Yoshinori Yasaka, M.D. Himeji Cardiovascular Center JapanDokument21 SeitenTips & Tricks of CTO PCI For Antegrade Approach: Yoshinori Yasaka, M.D. Himeji Cardiovascular Center JapanEll KlazureNoch keine Bewertungen