Beruflich Dokumente
Kultur Dokumente
Lecture 2 Burns
Hochgeladen von
Muhammad Shahzad Chandia0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
17 Ansichten18 SeitenE32
Originaltitel
Lecture 2 Burns - Copy
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenE32
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
17 Ansichten18 SeitenLecture 2 Burns
Hochgeladen von
Muhammad Shahzad ChandiaE32
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 18
The skin, the largest organ of the body
consists of two layers-the epidermis and dermis
.The depth or degree of burn depends on which layers of skin are damaged or
destroyed.
The epidermis is the outer layer that forms the protective covering.
The thicker or inner layer of the dermis contains blood vessels, hair follicles,
nerve endings, sweat and sebaceous glands.
When the dermis is destroyed, so are the nerve endings that allow a person to
feel pain, temperature, and tactile sensation.
The most important functions of the skin
Act as a barrier against infection.
The skin prevents loss of body fluids, thus preventing
dehydration.
The skin also regulates the body temperature by controlling
the amount of evaporation of fluids from the sweat glands.
The skin serves a cosmetic effect by giving the body shape.
When the skin is burned, these functions are impaired or lost
completely.
Burns occur when heat energy is applied at a faster rate
than tissue can absorb and dissipate it.
Fires, electric heating pads, hair dryers, scalding water,
steam, hot cooking oil, exhaust systems, and hot pipes
In man, temperatures above 113 F (45 C) can cause
coagulation necrosis and irreversible skin damage; a
temperature of 158 F (70 C) for only 1 second causes a
full-thickness burn
A transition zone separates completely devitalized tissue
from uninjured tissue
The transition zone is characterized by reduced blood
flow, intravascular sludging, and potentially reversible
tissue damage
It can be difficult to determine the burn depth and area of
involvement because the depth of injury is not uniform,
and the skin surface often is leathery and covered by dry
coagulum
CLASSIFICATION OF BURN
Superficial (first-degree) burns
Affect only epidermis.
Area is painful, thickened, erythematous, and desquamated.
Healing occurs rapidly (within 3 to 6 days) by
epithelialization from stratum germinativum or adnexal
dermal structures.
Dogs show less erythema with superficial burns than people
do.
Superficial partial thickness
They usually heal within 3 weeks because of
epithelialization from deeper portions of the skin appendages.
Healing usually is complete and occurs without grafting.
Deep partial-thickness (second-degree)
Cause major destruction of the dermis and upper layers of
the subcutaneous fat
Subcutaneous edema and notable inflammation occur
burns frequently heal without grafting, healing takes
months, and scarring may be extensive
Healing occurs by re-epithelialization from deep adnexa
and wound margins.
Ineffective therapy may allow a second-degree burn to
progress to a third-degree burn
Full-thickness (third-degree) burns
All skin structures are destroyed, and hair epilates easily
form a dark brown, insensitive, leathery eschar
Third-degree burns are less painful than first- or second-
degree burns because nerves have been destroyed
Early eschar removal is important as a necrotic eschar
quickly becomes colonized on its deep surface and serves
as a nidus of infection.
Burns that extend beyond the dermis are sometimes
classified as fourth-degree burns. They have the same
characteristics as third-degree burns but with additional
tissue damage extending into the muscle and bone.
Healing by secondary intention or reconstruction is usually
required.
TREATMENT
first priority in treating burns is to minimize tissue loss by
administering first aid and preventing shock
adequate perfusion, hydration, and wound protection
from trauma and infection may prevent progression of
tissue damage
Prevention of septic complications by good wound
management is the next priority
Cooling affected areas immediately after thermal injury
(within 2 hours) may limit extension of tissue destruction
Analgesics should be given as necessary to alleviate pain
Treatment cont
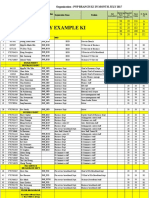
size of the burn area
a rough estimate can be gained using the rule of nine
each forelimb of the animal represents approximately 9%
of the total body surface area (TBSA); each rear limb is
18% (two nines); and the dorsal and ventral thorax and
abdomen are each 18%
Animals with partial-thickness burns involving less than
15% TBSA require minimal supportive therapy,
whereas those with burns involving more than 15% TBSA
require emergency supportive care
Treatment cont
Euthanasia should be considered for those with burns
involving more than 50% TBSA
The amount of isotonic fluid required during the first 24
hours may be estimated using the formula 3 to 4
ml/kg/percentage TBSA burned
Administration of protein colloids (i.e., fresh frozen
plasma or albumin) to hypoproteinemic patients should be
delayed for 8 to 12 hours to allow the stabilization of
membrane permeability and increased lymph return that
reduces protein loss
Transfusions (i.e., whole blood and packed red blood cells)
may be necessary in anemic patients.
Wound management
Removal of dead tissue is essential to the control of sepsis
and promotion of a viable vascular bed suitable for surgical
closure
Necrotic tissue may be dbrided from burn wounds with
dissection, autolytic, bandage
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- APMEPA Members ListDokument9 SeitenAPMEPA Members ListUsama100% (1)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Muhammad Usman Saleem (Standard Curve)Dokument3 SeitenMuhammad Usman Saleem (Standard Curve)Muhammad Shahzad ChandiaNoch keine Bewertungen
- Revised Syllabus CE-2016 10 Jul 2015Dokument158 SeitenRevised Syllabus CE-2016 10 Jul 2015Muhammad Faisal TahirNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shahzad Thesis Observation PerformaDokument1 SeiteShahzad Thesis Observation PerformaMuhammad Shahzad ChandiaNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Punjab Public Service CommissionDokument2 SeitenPunjab Public Service CommissionMuhammad Shahzad ChandiaNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Abdul Latif and Rafiq Cleaning Services L.L.CDokument2 SeitenAbdul Latif and Rafiq Cleaning Services L.L.CMuhammad Shahzad ChandiaNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- 66 CheeseDokument20 Seiten66 CheeselucasNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- 66 CheeseDokument20 Seiten66 CheeselucasNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- CV ShahzadDokument1 SeiteCV ShahzadMuhammad Shahzad ChandiaNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Veterinary ToxicologyDokument289 SeitenVeterinary ToxicologySamara Muniz100% (7)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Duck FarmingDokument52 SeitenDuck FarmingMuhammad Shahzad ChandiaNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- International Studentship Form v3.1Dokument2 SeitenInternational Studentship Form v3.1Muhammad Shahzad ChandiaNoch keine Bewertungen
- Common Lab TestsDokument2 SeitenCommon Lab TestsMuhammad Shahzad ChandiaNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Udder DevelopmentDokument45 SeitenUdder DevelopmentMuhammad Shahzad ChandiaNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Basic CVDokument1 SeiteBasic CVMuhammad Shahzad ChandiaNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Lecture 7 Aural HematomaDokument13 SeitenLecture 7 Aural HematomaMuhammad Shahzad ChandiaNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- 7 - Disorders of Urinary SystemDokument27 Seiten7 - Disorders of Urinary SystemMuhammad Shahzad ChandiaNoch keine Bewertungen
- Lecture 3, Skin GraftingDokument24 SeitenLecture 3, Skin GraftingZartasha KhanNoch keine Bewertungen
- Lecture 4 Dressing and BadageDokument20 SeitenLecture 4 Dressing and BadageMuhammad Shahzad ChandiaNoch keine Bewertungen
- Lecture 5 Lick GranulomaDokument7 SeitenLecture 5 Lick GranulomaMuhammad Shahzad ChandiaNoch keine Bewertungen
- CV IjazDokument1 SeiteCV IjazMuhammad Shahzad ChandiaNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- CV TemplateDokument2 SeitenCV TemplateMuhammad Shahzad ChandiaNoch keine Bewertungen
- Protrusion of The Third Eyelid GlandDokument14 SeitenProtrusion of The Third Eyelid GlandMuhammad Shahzad ChandiaNoch keine Bewertungen
- Lectue 16 Vaginal ProlapseDokument6 SeitenLectue 16 Vaginal ProlapseMuhammad Shahzad ChandiaNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Dr. Muhammad Shahzad Address: Basti Shahgarh P/O Mondka T/D Muzaffar Garh Mobile: (+923411678250) ProfileDokument3 SeitenDr. Muhammad Shahzad Address: Basti Shahgarh P/O Mondka T/D Muzaffar Garh Mobile: (+923411678250) ProfileMuhammad Shahzad ChandiaNoch keine Bewertungen
- Muhammad Shahzad: Special QualitiesDokument1 SeiteMuhammad Shahzad: Special QualitiesMuhammad Shahzad ChandiaNoch keine Bewertungen
- AmirDokument1 SeiteAmirMuhammad Shahzad ChandiaNoch keine Bewertungen
- Wound Between Fetlock and Pastern Joint and Maggots InfestationDokument17 SeitenWound Between Fetlock and Pastern Joint and Maggots InfestationMuhammad Shahzad ChandiaNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Production of YogurtDokument12 SeitenProduction of YogurtMuhammad Shahzad Chandia100% (1)
- Marine Cargo InsuranceDokument72 SeitenMarine Cargo InsuranceKhanh Duyen Nguyen HuynhNoch keine Bewertungen
- Artificial Intelligence Practical 1Dokument5 SeitenArtificial Intelligence Practical 1sadani1989Noch keine Bewertungen
- CAREDokument11 SeitenCARELuis SementeNoch keine Bewertungen
- Battery Checklist ProcedureDokument1 SeiteBattery Checklist ProcedureKrauser ChanelNoch keine Bewertungen
- June 2017 (IAL) MS - Unit 1 Edexcel Physics A-LevelDokument16 SeitenJune 2017 (IAL) MS - Unit 1 Edexcel Physics A-LevelNyraStardollNoch keine Bewertungen
- WBCS 2023 Preli - Booklet CDokument8 SeitenWBCS 2023 Preli - Booklet CSurajit DasNoch keine Bewertungen
- Changed Report 2015 PDFDokument298 SeitenChanged Report 2015 PDFAnonymous FKjeRG6AFnNoch keine Bewertungen
- Marketing Micro and Macro EnvironmentDokument8 SeitenMarketing Micro and Macro EnvironmentSumit Acharya100% (1)
- UAV Design TrainingDokument17 SeitenUAV Design TrainingPritam AshutoshNoch keine Bewertungen
- Caradol sc48 08Dokument2 SeitenCaradol sc48 08GİZEM DEMİRNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Philhis 1blm Group 6 ReportDokument19 SeitenPhilhis 1blm Group 6 Reporttaehyung trashNoch keine Bewertungen
- Reflection On The PoorDokument5 SeitenReflection On The Poorapi-347831792Noch keine Bewertungen
- Term Paper Inorganic PolymersDokument24 SeitenTerm Paper Inorganic PolymersCasey Karua0% (1)
- Nescom Test For AM (Electrical) ImpDokument5 SeitenNescom Test For AM (Electrical) Impشاہد یونسNoch keine Bewertungen
- Brahms Symphony No 4Dokument2 SeitenBrahms Symphony No 4KlausNoch keine Bewertungen
- Advertisement: National Institute of Technology, Tiruchirappalli - 620 015 TEL: 0431 - 2503365, FAX: 0431 - 2500133Dokument4 SeitenAdvertisement: National Institute of Technology, Tiruchirappalli - 620 015 TEL: 0431 - 2503365, FAX: 0431 - 2500133dineshNoch keine Bewertungen
- Enrico Fermi Pioneer of The at Ted GottfriedDokument156 SeitenEnrico Fermi Pioneer of The at Ted GottfriedRobert Pérez MartinezNoch keine Bewertungen
- Transparency and Digitalization in The Public Administration of RomaniaDokument8 SeitenTransparency and Digitalization in The Public Administration of RomaniaMădălina MarincaşNoch keine Bewertungen
- Electrical Engineering Lab Vica AnDokument6 SeitenElectrical Engineering Lab Vica Anabdulnaveed50% (2)
- Daewoo 710B PDFDokument59 SeitenDaewoo 710B PDFbgmentNoch keine Bewertungen
- 32 Hyderabad HITEC City BisleriDokument23 Seiten32 Hyderabad HITEC City BisleriSridhar ViswanathanNoch keine Bewertungen
- Web-Based Attendance Management System Using Bimodal Authentication TechniquesDokument61 SeitenWeb-Based Attendance Management System Using Bimodal Authentication TechniquesajextopeNoch keine Bewertungen
- C. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Dokument168 SeitenC. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Nelson100% (3)
- Paul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146Dokument27 SeitenPaul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146usman azharNoch keine Bewertungen
- Parallel Port Programming With DelphiDokument4 SeitenParallel Port Programming With Delphiramadhan1933Noch keine Bewertungen
- Additional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandDokument7 SeitenAdditional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandRizal TabootiNoch keine Bewertungen
- CTS2 HMU Indonesia - Training - 09103016Dokument45 SeitenCTS2 HMU Indonesia - Training - 09103016Resort1.7 Mri100% (1)
- PetrifiedDokument13 SeitenPetrifiedMarta GortNoch keine Bewertungen
- Hannah Mancoll - Research Paper Template - 3071692Dokument14 SeitenHannah Mancoll - Research Paper Template - 3071692api-538205445Noch keine Bewertungen
- PNP Ki in July-2017 AdminDokument21 SeitenPNP Ki in July-2017 AdminSina NeouNoch keine Bewertungen