Beruflich Dokumente
Kultur Dokumente
Parenteral and Enteral Nutrition in Neonate
Hochgeladen von
Anonymous N2PHMnTIYL0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
145 Ansichten22 SeitenOriginaltitel
Parenteral and Enteral Nutrition in Neonate.ppt
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
145 Ansichten22 SeitenParenteral and Enteral Nutrition in Neonate
Hochgeladen von
Anonymous N2PHMnTIYLCopyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 22
Parenteral and Enteral Nutrition
in Neonates
NICU Night Team Curriculum
Objectives
• Define basic nutritional requirements for neonatal growth
• Describe specific nutritional problems faced by low
birthweight and premature infants
• Know components and advantages of breastmilk;
indications for specific types of formulas
• Determine components of TPN and be able to write fluid
orders
• Formulate an individualized plan for starting and
advancing parenteral/enteral feeds
Goals of Nutrition
• To achieve a postnatal growth at a rate that
approximates the intrauterine growth of a normal fetus at
the same post-conceptional age
• Provide balance in fluid homeostasis and electrolytes
• Avoid imbalance in macro-nutrients
• Provide micro-nutrients and vitamins
Case
A 26 week female is born precipitously to a
healthy 20 year old G1P1 with an
uncomplicated pregnancy.
The baby is transferred to the NICU where a
UAC and UVC are placed. You are getting
ready to order fluids for this baby.
What is your goal growth for this infant?
What is this infant’s caloric requirement?
What fluids do you order?
Gastrointestinal Development
• Fetal swallowing, motility in 2nd trimester
– 18 week fetus swallows 18-50ml/kg/day
– Term 300-700ml/day
– Fetal swallowing regulates the volume of amniotic fluid and controls somatic
growth of the GI tract
• Intestines double in length from 25-40 weeks
• Functionally mature gut by 33-34 weeks
• Intestine in final anatomic position by 20 weeks
• Premature Infant GI tract:
– Delayed gastric emptying seen in preterm
• Breast milk, glucose polymers, prone positioning facilitate gastric emptying
– Total gut transit time in preterm 1-5 days
– Stooling delayed until after 3 days
– feeding volume ’s motility
Growth – General Facts
• Last trimester of pregnancy
– Fat and glycogen storing
– Iron reserves
– Calcium and phosphoruos deposits
• Premature babies more fluid (85%-95%), 10% protein,
0.1% fat.
– No glycogen stores
• The growth of VLBW infants lags considerably after birth
Growth Goals
• Weight: 20-30 g/day
• Length: ~1cm/week
• HC: 0.5cm/week
– Correlates with brain growth and later
development
Caloric Requirements for Growth
• Preterm goal: ~120kcal/kg/day
• Term goal: ~110kcal/kg/day
• Total Fluid of enteral feeds required to
deliver adequate calories for growth is
~150cc/kg/day
Total Parenteral Nutrition
Determine fluid requirement (mL/kg/day) for first
day of life
Full-term infants: 60–80 mL/kg/day
Late preterm and preterm infants (30–37 weeks): 80 mL/kg/day
Very-preterm infants: 100–120 mL/kg/day
Determine Glucose Infusion Rate (GIR)
GIR: (% dextrose x IV rate ) ÷ (6 x wt in kg) Calculate GIR from
known dextrose concentration (%).
Example: An infant weighs 2 kg and is receiving 100
ml/kg/day of dextrose 15% solution.
– IV rate: 100 × 2 = 200 ml/day ÷ 24 = 8.3 ml/hr
– GIR: (15% x 8.3 x 0.1667) ÷ 2 = 10.3mg/kg/min
(15% x 8.3 ) ÷ (6 x 2) = 10.3 mg/kg/min
Total Parenteral Nutrition
Protein and amino acids
• Start with 2- 3 g/kg/day
– Increase 0.5–1.5 g/kg/day to a total of 3–4 mg/kg/day
• Goal for premature infants: 4g/kg/day
• Goal for term infants: 3g/kg/day
• Source: trophamine
Calculate electrolytes to add to bag
• DOL#1: dextrose in water with no eletrolutes is usually appropriate except in
premies with low Ca stores who may require Ca
• DOL#2: add electrolytes to the bag based on estimated daily requirements and
BMP
– Estimated Needs:
• NaCl = 2-4 mEq/kg/day
• KCl = 1-2 mEq/kg/day (NOTE: Do not supplement K until UOP >1cc/kg/hr, especially in
premies)
• CaGluconate =200-400mg/kg/day (NOTE: mg not mEq and Ca cannot be infused at
>200mg/kg/day through a central line)
Total Parentral Nutrition
Other added nutrients
• Lipids
• Cystein
• Phosphrous
• Magnesium
• Trace Minerals
• MVI
• Heparin
Central TPN Peripheral TPN
• Easy to meet nutrition needs – Unable to meet needs for
• No limits on osmolarity Ca/Phos needs
• Little risk of phlebitis – Maximum rate of Calcium
• Long term use gluconate is 200mg/kg/d
• May require general anesthesia – Maximum % dextrose is
• Greater risk of infection 12.5%
• Increased cost – Short term use
• Greater risk of mechanical injury, – Less risk for catheter related
air embolism, venous obstruction infections
– Lower cost ?
– Less risk of mechanical injury,
air embolism, venous
obstruction
Total Parenteral Nutrition
Enteral Nutrition
• Breast milk is best!
• The American Academy of Pediatrics (2005) recommends
breastfeeding for the first year of life.
• Started when an infant is clinically stable
• Absence of food in the GI tract produces mucosal and villous
atrophy and reduction of enzymes necessary for digestion and
substrate absorption
• Trophic hormones normally produced in the mouth, stomach, and
gut in response to enteral feeding are diminished.
• Breastmilk and standard infant formula have 20kcal/30cc
(30cc=1oz)
• Specialized formulas and fortifiers allow caloric content to be
increased
Breastmilk
• Preferred source of enteral nutrition
• Very well tolerated by most infants
• Improves gastric emptying time
• Matures the mucosal barrier
• Promotes earlier & appearance of IgA
• Vastly ’s incidence of NEC
• More significant induction of lactase activity compared to formula fed
premies
• Composition:
– Varies with gestation
– Varies according to maternal diet
– Varies within a feeding( fat in last ½ fdg)
– Varies within the day( fat in PM over AM)
Enteral Nutrition in the NICU
• Term:
– If clinically stable, start PO ad lib feeds and advance as
tolerated
• Preterm
– Feeds are often initiated with breastmilk, Sim 20 or SSC
24
– Trophic tube feeds may be continuous or bolus and
advanced gradually (10-20mL/kg/day)
– Transition to bolus from continuous typically begins after
achieving full feeds
– PO feeds typically attempted around 32-34 weeks, when
premies develop suck and swallow coordination
– Premies are often supplemented with TPN as they work
up on feeds
– Goal discharge formula is Neosure 22
What to Feed?
What to Feed?
Practice Problems
Baby boy B weighs 1.2 kg. The IV rate is 6.8 ml/hr, and the IV fluid
contains the following:
• 1.5 mEq of sodium per 100 ml
• 1.9 mEq of potassium per 100 ml
• 3.0 mEq of calcium per 100 ml
• 1.2 mMol of phosphorus per 100 ml.
Calculate the amount of sodium/kg/day, potassium/kg/day,
calcium/kg/day, and phosphorus/kg/day that baby boy B is
receiving.
Answer:
• 2 mEq of sodium/kg/day
• 2.6 mEq of potassium/kg/day
• 4.1 mEq of calcium/kg/day
• 1.6 mMol of phosphorus/kg/day
Practice Problems
Baby boy C weighs 1.5 kg. Total IV fluids are to be
calculated at 140 ml/kg/day. The infant is receiving
central TPN. Lipids are 2 gram/kg/day.
Write TPN orders (including dextrose concentration and IV
rates) to give baby C a glucose infusion rate of 8
mg/kg/min.
Write orders for 4 mEq/kg of sodium, 2 mEq/kg of
potassium, 3.5 mEq of calcium, and 1.5 mMol of
phosphorus to be added to every 100 ml of IV base
solution.
Answer:
• Lipids: 0.6 ml/hr
• PN fluids: dextrose 8.9% at 8.1 ml/hr
• Sodium: 3.1 mEq per 100 ml
• Potassium: 1.5 mEq per 100 ml
• Calcium: 2.7 mEq per 100 ml
• Phosphorus: 1.1 mMol per 100 ml
References
• American Academy of Pediatrics, Section on Breastfeeding. (2005). Policy statement: Breastfeeding and the use of
human milk. Pediatrics, 115(2), 496–506.
• Carlson, C, Shirland, S. Neonatal Parenteral and Enteral Nutrition, Resource Guide. National Association of Neonatal
Nurse Practitioners
• Adamkin, D. Nutrition Management of the Very Low-birthweight Infant: I. Total Parenteral Nutrition and Minimal
Enteral Nutrition. NeoReviews 2006;7;e602-e607
• Hay, W. Strategies for Feeding the Preterm Infant. Neonatology. 2008 ; 94(4): 245–254.
Thank you NNPs Carol and Terri!
Das könnte Ihnen auch gefallen
- Kuliah Blok Growth and DevelopmentDokument44 SeitenKuliah Blok Growth and Developmentjaish8904Noch keine Bewertungen
- NICU Nutrition GuideDokument22 SeitenNICU Nutrition GuideStrept PneumoniaNoch keine Bewertungen
- Neonatal TPN: Dr. Fahad Al-AqlDokument10 SeitenNeonatal TPN: Dr. Fahad Al-AqlAnonymous 9dVZCnTXSNoch keine Bewertungen
- Parenteral Nutrition (PN) Clinical and Practical Considerations - CompressedDokument53 SeitenParenteral Nutrition (PN) Clinical and Practical Considerations - CompressedFiya AwanNoch keine Bewertungen
- Neonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualDokument7 SeitenNeonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualNugraha SultanNoch keine Bewertungen
- Principle of Pediatric Nutrition Care For ConsultantDokument17 SeitenPrinciple of Pediatric Nutrition Care For ConsultantvivydesyantiNoch keine Bewertungen
- Pediatric Nutritional AssessmentDokument51 SeitenPediatric Nutritional Assessmentcharanjit kaur100% (1)
- Medical Nutrition Therapy For Paediatric ConditionsDokument57 SeitenMedical Nutrition Therapy For Paediatric ConditionsﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞNoch keine Bewertungen
- Nutrition Intervention - What's AvailableDokument39 SeitenNutrition Intervention - What's AvailablesitihawamtNoch keine Bewertungen
- Managing Diabetes Through Proper Treatment and MonitoringDokument10 SeitenManaging Diabetes Through Proper Treatment and Monitoringjoeln_9Noch keine Bewertungen
- Drug-Nutrient Interaction in Prescriptions ForDokument7 SeitenDrug-Nutrient Interaction in Prescriptions ForRafika DitaNoch keine Bewertungen
- Nutritional AssessmentDokument7 SeitenNutritional AssessmentSaher YasinNoch keine Bewertungen
- Session 2 Basics of NutritionDokument39 SeitenSession 2 Basics of NutritionAllyeah bethel GrupoNoch keine Bewertungen
- Nutrition Care Process Note-IcuDokument2 SeitenNutrition Care Process Note-Icuapi-1032325430% (1)
- Severe Acute Malnutrition and Fluid Management inDokument76 SeitenSevere Acute Malnutrition and Fluid Management inBibsNoch keine Bewertungen
- Nutrition - TPN (Basics)Dokument37 SeitenNutrition - TPN (Basics)Giorgi BradNoch keine Bewertungen
- 24 HR Food RecallDokument39 Seiten24 HR Food RecallKon Zhen JieNoch keine Bewertungen
- 406 ReflectionDokument1 Seite406 Reflectionapi-533641139Noch keine Bewertungen
- Parenteral Nutrition: Indications and RequirementsDokument56 SeitenParenteral Nutrition: Indications and RequirementsdenekeNoch keine Bewertungen
- Operational Guidelines Acute Malnutrition South Africa FINAL-1!8!15-2Dokument70 SeitenOperational Guidelines Acute Malnutrition South Africa FINAL-1!8!15-2RajabSaputra100% (2)
- Nutritional Disorders in Filipino ChildrenDokument9 SeitenNutritional Disorders in Filipino ChildrenJill Sanchez-SadiaNoch keine Bewertungen
- Medicine and Nutrition Case StudyDokument5 SeitenMedicine and Nutrition Case Studyapi-384113918Noch keine Bewertungen
- Nutrition PaperDokument4 SeitenNutrition Paperapi-433705780Noch keine Bewertungen
- Health Assessment AssignmentDokument8 SeitenHealth Assessment Assignmentapi-314827222100% (1)
- Nutrition Management Premie NashDokument49 SeitenNutrition Management Premie NashathaNoch keine Bewertungen
- Vitamin B12 Deficiency and A Patient Case StudyDokument36 SeitenVitamin B12 Deficiency and A Patient Case Studynherm6425100% (1)
- PES StatementsDokument6 SeitenPES Statementsdoniazad13112Noch keine Bewertungen
- Unani Medicine for IBSDokument26 SeitenUnani Medicine for IBSDr. Md. Shahab UddinNoch keine Bewertungen
- PN Monitoring and ComplicationsDokument35 SeitenPN Monitoring and ComplicationsRhomizal Mazali100% (1)
- Nutrition Care Process WorksheetDokument7 SeitenNutrition Care Process Worksheetapi-338119904Noch keine Bewertungen
- Complementary FeedingDokument38 SeitenComplementary FeedingsitihawamtNoch keine Bewertungen
- Diet TherapyDokument140 SeitenDiet Therapyraghadalesawi51Noch keine Bewertungen
- Nutritional DisordersDokument50 SeitenNutritional Disorderstayyab khanNoch keine Bewertungen
- Medical Nutrition Therapy For DiabetesDokument27 SeitenMedical Nutrition Therapy For DiabetesAlfitri YuniNoch keine Bewertungen
- Dietary Intake AssessmentDokument4 SeitenDietary Intake AssessmentMary Mae BuellaNoch keine Bewertungen
- Nutritional Issues in The ICU Case FileDokument2 SeitenNutritional Issues in The ICU Case Filehttps://medical-phd.blogspot.com100% (1)
- Nutrition During LactationDokument25 SeitenNutrition During LactationDaniel HeryantoNoch keine Bewertungen
- Hospital DietsDokument1 SeiteHospital DietsAnne Julia AgustinNoch keine Bewertungen
- Nutrition: - . - and The Surgical Patient (Pre and Post Operative Nutrition)Dokument58 SeitenNutrition: - . - and The Surgical Patient (Pre and Post Operative Nutrition)SanaSofiyahNoch keine Bewertungen
- Essential Enteral and Parenteral Nutrition GuideDokument64 SeitenEssential Enteral and Parenteral Nutrition GuideHeba IyadNoch keine Bewertungen
- The Registered Dietitian: Perceptions, Assumptions, and RealityDokument50 SeitenThe Registered Dietitian: Perceptions, Assumptions, and RealityARKressNoch keine Bewertungen
- Nutrition in ICU: DR Rahul VarshenyDokument50 SeitenNutrition in ICU: DR Rahul VarshenyAntar InenigogNoch keine Bewertungen
- MNT for Diabetes Nutrition TherapyDokument27 SeitenMNT for Diabetes Nutrition Therapydr.Uci BaharNoch keine Bewertungen
- Public Health NutritionDokument58 SeitenPublic Health NutritionJaime TaylorNoch keine Bewertungen
- Pes Statements SamplesDokument19 SeitenPes Statements SamplesJennie ManobanNoch keine Bewertungen
- Case Study 19Dokument3 SeitenCase Study 19api-533641139Noch keine Bewertungen
- Nutr 510 - Counseling Session 2Dokument4 SeitenNutr 510 - Counseling Session 2api-240740872Noch keine Bewertungen
- Low Birthweight InfantDokument42 SeitenLow Birthweight InfantJoNoch keine Bewertungen
- 12 Neonatal Hypocalcemia, Glycemia and MagnesemiaDokument55 Seiten12 Neonatal Hypocalcemia, Glycemia and MagnesemiaRana Vandana100% (1)
- Energy Intake and ExpenditureDokument38 SeitenEnergy Intake and ExpenditureNichNoch keine Bewertungen
- Protocal Followed For Enteral FeedingDokument4 SeitenProtocal Followed For Enteral FeedingK Jayakumar KandasamyNoch keine Bewertungen
- Katherine Orourke Resume With ReferencesDokument2 SeitenKatherine Orourke Resume With Referencesapi-485480196Noch keine Bewertungen
- Nurses' Role in Nutrition and DieteticsDokument53 SeitenNurses' Role in Nutrition and DieteticsLouie ParillaNoch keine Bewertungen
- Enteral Nutrition Manual Oct 2011Dokument51 SeitenEnteral Nutrition Manual Oct 2011Salilah Mahfudz100% (1)
- Total Parenteral Nutrition:: By: Group 4Dokument25 SeitenTotal Parenteral Nutrition:: By: Group 4Mylz MendozaNoch keine Bewertungen
- Safe Upper Levels For Vitamins and Minerals (FSA)Dokument360 SeitenSafe Upper Levels For Vitamins and Minerals (FSA)jcpchin2Noch keine Bewertungen
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionVon EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNoch keine Bewertungen
- Guidelines for Measuring Household and Individual Dietary DiversityVon EverandGuidelines for Measuring Household and Individual Dietary DiversityNoch keine Bewertungen
- Obstetrics Study Guide on Hypertension, Preterm Labor, InfectionDokument172 SeitenObstetrics Study Guide on Hypertension, Preterm Labor, InfectionAnonymous N2PHMnTIYLNoch keine Bewertungen
- PPROMDokument55 SeitenPPROMAnonymous N2PHMnTIYLNoch keine Bewertungen
- FertilisasiDokument18 SeitenFertilisasiAnonymous N2PHMnTIYLNoch keine Bewertungen
- Kuliah Blok 2 Gangguan Hemodinamik Trombosis Dan ShockDokument37 SeitenKuliah Blok 2 Gangguan Hemodinamik Trombosis Dan ShockAnonymous N2PHMnTIYLNoch keine Bewertungen
- What Did You Learn Tuday Dear Indira Cari PentingDokument1 SeiteWhat Did You Learn Tuday Dear Indira Cari PentingAnonymous N2PHMnTIYLNoch keine Bewertungen
- Curriculum Vitae: Personal IdentificationDokument2 SeitenCurriculum Vitae: Personal IdentificationAnonymous N2PHMnTIYLNoch keine Bewertungen
- Belajar Bahasa InggrisDokument2 SeitenBelajar Bahasa InggrisAnonymous N2PHMnTIYLNoch keine Bewertungen
- What Did You Learn Tuday Dear Indira Cari PentingDokument1 SeiteWhat Did You Learn Tuday Dear Indira Cari PentingAnonymous N2PHMnTIYLNoch keine Bewertungen
- Banana - Recommendations For Maintaining Postharvest Quality - Postharvest Technology Center - UC Davis PDFDokument3 SeitenBanana - Recommendations For Maintaining Postharvest Quality - Postharvest Technology Center - UC Davis PDFFernando SanchezNoch keine Bewertungen
- FOI Research On AcupunctureDokument118 SeitenFOI Research On AcupunctureDilutionsUKNoch keine Bewertungen
- Proliferation Therapy for Tendon and Ligament InjuriesDokument18 SeitenProliferation Therapy for Tendon and Ligament InjuriesJason Tutt GinNoch keine Bewertungen
- Department Check List Final 3Dokument27 SeitenDepartment Check List Final 3BOOKREADER_NOWNoch keine Bewertungen
- FMST 314 Finals NotesDokument8 SeitenFMST 314 Finals NotesmoomoomaoNoch keine Bewertungen
- Parkinson DiseaseDokument9 SeitenParkinson DiseaseMarco GunawanNoch keine Bewertungen
- IHI Global Trigger ToolDokument46 SeitenIHI Global Trigger ToolJuan Manuel LujanNoch keine Bewertungen
- Narrative TherapyDokument11 SeitenNarrative TherapyCamila Orellana100% (1)
- Ot ProtocolDokument38 SeitenOt ProtocolSelva KumarNoch keine Bewertungen
- Categories of Disability Under IDEADokument6 SeitenCategories of Disability Under IDEANational Dissemination Center for Children with DisabilitiesNoch keine Bewertungen
- CTCAE 4.03 2010-06-14 QuickReference 5x7Dokument196 SeitenCTCAE 4.03 2010-06-14 QuickReference 5x7Andreea ZaharieNoch keine Bewertungen
- Treatment of Pregnancy-Related Lumbar and Pelvic Girdle Pain by The Yoga Method: A Randomized Controlled StudyDokument8 SeitenTreatment of Pregnancy-Related Lumbar and Pelvic Girdle Pain by The Yoga Method: A Randomized Controlled StudyJosephineeNoch keine Bewertungen
- Fred Maiorino CaseDokument11 SeitenFred Maiorino CaseGajo VankaNoch keine Bewertungen
- Chapter 4 - P4 P5 The Role of Complementary TherapiesDokument8 SeitenChapter 4 - P4 P5 The Role of Complementary TherapiesdesbestNoch keine Bewertungen
- 7th Panhellenic Congress of Thermal MedicineDokument6 Seiten7th Panhellenic Congress of Thermal MedicineEmmanuel Manolis KosadinosNoch keine Bewertungen
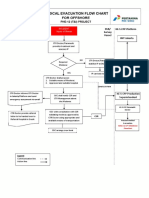
- 3-A4 - Medical Evacuation Flow Chart (Rev.0)Dokument1 Seite3-A4 - Medical Evacuation Flow Chart (Rev.0)SiskaNoch keine Bewertungen
- HeelDokument4 SeitenHeelDoha EbedNoch keine Bewertungen
- Platelet-Rich Plasma For Hair Restoration: Natalie Justicz,, Adeeb Derakhshan,, Jenny X. Chen,, Linda N. LeeDokument7 SeitenPlatelet-Rich Plasma For Hair Restoration: Natalie Justicz,, Adeeb Derakhshan,, Jenny X. Chen,, Linda N. Leejaviers45Noch keine Bewertungen
- ArdsDokument29 SeitenArdsAmani KayedNoch keine Bewertungen
- Water Supply and Sanitary Engineering by Chittaranjan Bibhar 2cfa37 PDFDokument115 SeitenWater Supply and Sanitary Engineering by Chittaranjan Bibhar 2cfa37 PDFRahul TomarNoch keine Bewertungen
- Final Submission UpdatedDokument26 SeitenFinal Submission Updatedapi-528981305Noch keine Bewertungen
- Antenatal CareDokument4 SeitenAntenatal Caredrfaruqui2551100% (1)
- Adrenal Care ShaktiDokument12 SeitenAdrenal Care ShaktiAnonymous 7R6n0f9BY100% (2)
- Case Presentation BronchiectasisDokument61 SeitenCase Presentation BronchiectasisUzair Muhd100% (6)
- Tress Test: The Gale Encyclopedia of MedicineDokument7 SeitenTress Test: The Gale Encyclopedia of MedicineSalsabilla KimikoNoch keine Bewertungen
- Neonatal Resuscitation Power PointDokument29 SeitenNeonatal Resuscitation Power PointsameerarswNoch keine Bewertungen
- Intramuscular CKLDokument2 SeitenIntramuscular CKLapi-310181843Noch keine Bewertungen
- Quinine 1Dokument3 SeitenQuinine 1Vhan BetizNoch keine Bewertungen
- PsychopathiaDokument26 SeitenPsychopathiaKunal KejriwalNoch keine Bewertungen
- Test Bank For Maternal Child Nursing 5th EditionDokument8 SeitenTest Bank For Maternal Child Nursing 5th EditionJennifer Burke100% (34)