Beruflich Dokumente
Kultur Dokumente
BMW
Hochgeladen von
Pabhat Kumar100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
463 Ansichten24 Seitenbmw..poerpoikj
Originaltitel
BMW ppt
Copyright
© © All Rights Reserved
Verfügbare Formate
PPTX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenbmw..poerpoikj
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
463 Ansichten24 SeitenBMW
Hochgeladen von
Pabhat Kumarbmw..poerpoikj
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 24
Biomedical waste management
Presented by: Mahusmita Naik
Sushruta Mohapatra
Itismita Biswal
Sandhya Sahoo
Definition:
According to Biomedical Waste (Management and
Handling) Rules, 1998 of India “Any waste which is
generated during the diagnosis, treatment or
immunization of human beings or animals or in
research activities pertaining there to or in the
production or testing of bio medicals.
OR
According to WHO, the waste generated during the
diagnosis,testing, treatment, research or
production of biological products for humans or
animals.
Importance of biomedical waste
management:
• To protect the environment .
• For the health & Safety of the Population.
TYPE OF HOSPITAL WASTE
1. Non-hazardous waste:-
• Biodegradable
• Non- Biodegradable
2. Potentially infectious waste;- Dressings, swabs, laboratory
wastes, instruments used in patient care.
3. Potentially toxic waste:-
• Radioactive :- Radiotherapy/lab research liquids
Contaminated glass wares, packages, absorbent papers
• Chemical :- Lab reagents , Film developer, Expired
disinfectants, Expired solvents
• Pharmaceutical:- Expired Pharmaceuticals, Contaminated
Pharmaceuticals, Banned Pharmaceuticals
SEGREGATION, TRANSPORTATION &
DISPOSAL OF BIO-MEDICAL WASTE
• No untreated bio-medical waste shall be mixed with
other wastes.
• The bio-medical waste shall be segregated into containers
or bags at the point of generation prior to its storage,
transportation, treatment and disposal.
• The containers or bags are according to the type of Bio-
medical waste.
• The operator of common bio-medical waste treatment
facility shall transport the bio-medical waste from the
premises of hospital to any off-site bio-medical waste
treatment facility only in the vehicles having label along
with necessary information of segregation of Bio-medical
waste
Cont…
• The vehicles used for transportation of bio-
medical waste should be a covered trolly.
• It transport bio-medical waste usually at morning
6am & evening 4pm( especially when there is not
busy schedule)
• Microbiology waste and all other clinical
laboratory waste shall be pre-treated by
sterilisation or disinfection as per the World
Health Organisation guidelines before packing
and sending to the common bio-medical waste
treatment facility.
cont….
• Untreated human anatomical waste, animal
anatomical waste, soiled waste and,
biotechnology waste shall not be stored
beyond a period of 48hrs.
DECONTAMINATION OF BMW
• Decontamination is the process whereby microbial
contamination of a material is reduced to render it
safe to handle. There are two methods of achieving
this, disinfection and sterilisation, which are used in
hospitals.
• The combination of processes (including cleaning,
disinfection and sterilisation) used to render a re-
usable item safe for further use on patients and
handling by staff. Effective decontamination is
essential in reducing the risk of transmission of
infectious agents. In the decontamination process
soiled instruments are stored, inspected and if
necessary, disassembled.
Disinfection
• It is the process of partial removal or destruction of
organisms except spores.
• Disinfection refers to a treatment that is designed
to reduce the potential infectivity of a material to a
level that effectively destroys its potential to cause
harm. It does not necessarily remove all viable
micro-organisms.
• Chemical disinfection should be used routinely for
decontamination of discarded liquid cultures,
possibly small amounts of solid material (e.g. small
sample tubes), surfaces and spillages.
Types of disinfectants
• Aldehyde mainly gluteraldehyde
Formaldehyde ◦ should only be used for
fumigation of laboratories
• Alcohol
• Virkon is often the disinfectant of choice in
laboratories due to its wide spectrum of
activity and less hazardous properties
Sterilization:
• It is the process used to render an object free
from all organisms including spores.
• Sterilisation is best practice for inactivating
biological waste and is defined as effectively
giving a 100% kill.
• The Sterile Processing Department (SPD), also
known as the Central Sterile Services
Department (CSSD), is the area in a hospital
where cleaning and sterilization of devices used
in medical procedures takes place.
Process of sterilization:
• Soiled instruments from the operating
room are first taken to the
decontamination area to be cleaned of
gross soils and inspected for damage.
• The Instruments are first manually
cleaned. Depending on the device, they
may then go through an automated
washing process following manual
cleaning.
Cont…
• Manual cleaning requires either a two-bay sink
or three-bay sink. In a three-sink method, each
bay plays a role in the cleaning process.
• Sink 1: Instruments are immersed in an
enzymatic solution to begin breaking down soils
• Sink 2: Instruments are immersed in a detergent
solution and manually brushed
• Sink 3: Instruments are thoroughly rinsed with
clean, treated water
Methods of sterilization:
• Reliable sterilization depends on contact of the
sterilizing agent with all surfaces of the item to be
sterilized.
Steam
• Heat destroys microorganisms, but this process is
hastened by the addition of moisture.
• Pressure, greater than atmospheric, is necessary to
increase the temperature of steam for thermal
destruction of microbial life.
• Death by moist heat in the form of steam under
pressure is caused by the denaturation and coagulation
of protein or the enzyme-protein system within the
cells.
• Exposure time depends upon size and contents of load,
and temperature within the sterilizer.
Ethylene Oxide
• Ethylene oxide is used to sterilize items that
are heat or moisture sensitive.
• Ethylene oxide (EO) is a chemical agent that
kills microorganisms, including spores, by
interfering with the normal metabolism of
protein and reproductive, processes,
resulting in death of cells.
Dry heat
• Dry heat in the form of hot air is used
primarily to sterilize anhydrous oils,
petroleum products, and bulk powders that
steam and ethylene oxide gas cannot
penetrate.
• Death of microbial life by dry heat is a
physical oxidation or slow burning process of
coagulating the protein in cells.
Formaldehyde gas
• Formaldehyde kills microorganisms by
coagulation of protein in cells.
• Used as a fumigant in gaseous form,
formaldehyde sterilization is complex and less
efficacious than other methods of sterilization.
Microwaves
• The nonionizing radiation of microwaves
produces hyperthermic conditions that disrupt
life processes.
• This heating action affects water molecules and
interferes with cell membranes.
• Microwave sterilization uses low-pressure steam
with the nonionizing radiation to produce
localized heat that kills microorganisms.
Hydrogen peroxide
• Hydrogen peroxide is activated to create a
reactive plasma or vapor.
• The plasma and vapor phases of hydrogen
peroxide are highly sporicidal even at low
concentrations and temperature.
Summary
Das könnte Ihnen auch gefallen
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesVon EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNoch keine Bewertungen
- Universal PrecautionDokument10 SeitenUniversal PrecautionParth VasaveNoch keine Bewertungen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- CVP MonitoringDokument24 SeitenCVP MonitoringChoji Heiwajima100% (1)
- Alexander FlemingDokument9 SeitenAlexander FlemingEdwin Donny YahyaNoch keine Bewertungen
- Sterilization and DisinfectionDokument68 SeitenSterilization and DisinfectionMohammed Qasim Al-WataryNoch keine Bewertungen
- Inflamation AssignmentDokument59 SeitenInflamation AssignmentAnonymous GRUjCVedhNoch keine Bewertungen
- ANAMEIA PPT BY SandeepDokument32 SeitenANAMEIA PPT BY SandeepSandeep ChakravarthyNoch keine Bewertungen
- Identification of Microorganisms: Unknown SpecimensDokument10 SeitenIdentification of Microorganisms: Unknown SpecimensAnonymous wVgEAr6Noch keine Bewertungen
- Nosocomial Infection?Dokument4 SeitenNosocomial Infection?Sara ANoch keine Bewertungen
- Antiadrenergic Drugs 23.07.018 PDFDokument23 SeitenAntiadrenergic Drugs 23.07.018 PDFHitesh karnNoch keine Bewertungen
- AnthopometryDokument44 SeitenAnthopometryghifari2007Noch keine Bewertungen
- Changing Trend in Hospitalization Old ConceptsDokument8 SeitenChanging Trend in Hospitalization Old ConceptsMakhanVermaNoch keine Bewertungen
- InhalDokument33 SeitenInhallupeNoch keine Bewertungen
- Diagnosi S: MalariaDokument28 SeitenDiagnosi S: MalariaOm Prakash SinghNoch keine Bewertungen
- Management of Pregnancy JaundiceDokument28 SeitenManagement of Pregnancy JaundiceShailani Thakur100% (1)
- Tuberculosis Unit 1 Lecture - 1Dokument39 SeitenTuberculosis Unit 1 Lecture - 1Kubra Rasool100% (1)
- Community Health One LinersDokument30 SeitenCommunity Health One LinersRatan YadavNoch keine Bewertungen
- Drug Used in Skin and Mucus MembraneDokument35 SeitenDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Admission and EmergencyDokument12 SeitenAdmission and EmergencyRashid AyubiNoch keine Bewertungen
- (Pelvic Inflammatory Disease) Samiya AhmedDokument31 Seiten(Pelvic Inflammatory Disease) Samiya AhmedSaamiya AhmedNoch keine Bewertungen
- Esophageal CancerDokument25 SeitenEsophageal CancerK poojithaNoch keine Bewertungen
- Q Oral Glucose Tolerance TestDokument4 SeitenQ Oral Glucose Tolerance TestNur Amirah FarhanahNoch keine Bewertungen
- Fluid and Electrolyte Imbalance and Nutritional ProblemDokument98 SeitenFluid and Electrolyte Imbalance and Nutritional ProblemPaul EbenezerNoch keine Bewertungen
- Blood CoagulationDokument10 SeitenBlood CoagulationgauravkokraNoch keine Bewertungen
- 847 - Protein Energy MalnutritionDokument20 Seiten847 - Protein Energy MalnutritionPriyanka Vikas TakNoch keine Bewertungen
- Standard Precautions PolicyDokument8 SeitenStandard Precautions PolicyMasrov TukirovNoch keine Bewertungen
- Needle Cricothyroidotomy 2 - Hatem AlsrourDokument32 SeitenNeedle Cricothyroidotomy 2 - Hatem Alsrourhatem alsrour100% (2)
- Anti Malarial DrugsDokument107 SeitenAnti Malarial DrugsSindile MchunuNoch keine Bewertungen
- Approach To An Unconscious Patient-OyeyemiDokument41 SeitenApproach To An Unconscious Patient-OyeyemiOyeyemi AdeyanjuNoch keine Bewertungen
- N7 by Novo - Methods of ContraceptionDokument34 SeitenN7 by Novo - Methods of ContraceptionEllen Rose NovoNoch keine Bewertungen
- Somatosensory System OkDokument47 SeitenSomatosensory System OkIrayumastutiNoch keine Bewertungen
- Goitre: Dr. Sandhya Gupta Assistant Professor General SurgeryDokument59 SeitenGoitre: Dr. Sandhya Gupta Assistant Professor General SurgerySandhya guptaNoch keine Bewertungen
- Triage in Disaster ManagementDokument10 SeitenTriage in Disaster ManagementHazel Mei MalvarNoch keine Bewertungen
- Infection Control MCQDokument3 SeitenInfection Control MCQJaindra NaroliaNoch keine Bewertungen
- Corneal UlcersDokument18 SeitenCorneal UlcersAvinash NagarNoch keine Bewertungen
- Protein Energy Malnutrition - 2Dokument32 SeitenProtein Energy Malnutrition - 2J V SamuelNoch keine Bewertungen
- NephritisDokument21 SeitenNephritisruchikaNoch keine Bewertungen
- NEPHROSISDokument31 SeitenNEPHROSISvinnu kalyanNoch keine Bewertungen
- Universal Immunization ProgrammeDokument8 SeitenUniversal Immunization ProgrammeNagaraj ReddyNoch keine Bewertungen
- ARDS Care Respiratory Care Plan PDFDokument2 SeitenARDS Care Respiratory Care Plan PDFeric parlNoch keine Bewertungen
- Anti-Tubercular Drugs Classification and MechanismDokument88 SeitenAnti-Tubercular Drugs Classification and MechanismEscitalopram 5mgNoch keine Bewertungen
- Graft RejectionDokument33 SeitenGraft Rejectionasmaa100% (1)
- Osh State UniversityDokument14 SeitenOsh State Universitykhuzaima9Noch keine Bewertungen
- Morphology and Classification of Bacteria - SundarDokument25 SeitenMorphology and Classification of Bacteria - SundarNithin SundarNoch keine Bewertungen
- SalmonellaDokument27 SeitenSalmonellaDayana PrasanthNoch keine Bewertungen
- Medical Diseases Complicating Pregnancy: by The Name of AllahDokument45 SeitenMedical Diseases Complicating Pregnancy: by The Name of Allah'محمد علي' محمد لافيNoch keine Bewertungen
- Disinfection and SterilisationDokument36 SeitenDisinfection and SterilisationvaidyamNoch keine Bewertungen
- HypertensionDokument21 SeitenHypertensionM RaisNoch keine Bewertungen
- Essential Newborn CareDokument67 SeitenEssential Newborn CareTadesse MuhammedNoch keine Bewertungen
- Ectopic PregnancyDokument76 SeitenEctopic PregnancyVivian Jean TapayaNoch keine Bewertungen
- Handling and care of experimental animalsDokument26 SeitenHandling and care of experimental animalsABHINABA GUPTANoch keine Bewertungen
- 1593983660haemoglobin Estimation MethodsDokument24 Seiten1593983660haemoglobin Estimation MethodsJune VasquezNoch keine Bewertungen
- Oxygen Therapy and Oxygen Delivery (Pediatric) - CEDokument8 SeitenOxygen Therapy and Oxygen Delivery (Pediatric) - CEViviana AltamiranoNoch keine Bewertungen
- CSOM TreatmentDokument21 SeitenCSOM TreatmentSarwinder SinghNoch keine Bewertungen
- Interpretation of Clinical Biochemical TestsDokument24 SeitenInterpretation of Clinical Biochemical TestsaddwrNoch keine Bewertungen
- Iv TherapyDokument3 SeitenIv TherapylovlyNoch keine Bewertungen
- Anemia: Presented byDokument36 SeitenAnemia: Presented byParmvir Singh100% (1)
- Post Operative HemorrhageDokument16 SeitenPost Operative Hemorrhagenishimura89Noch keine Bewertungen
- Rheumatic Fever: DR: Kaem Shir AliDokument24 SeitenRheumatic Fever: DR: Kaem Shir AliMwanja Moses100% (1)
- Kangaroo Mother Care: Dr. Maheswari JaikumarDokument67 SeitenKangaroo Mother Care: Dr. Maheswari JaikumarMeena KoushalNoch keine Bewertungen
- PPTCT Policy Guideline PDFDokument31 SeitenPPTCT Policy Guideline PDFPabhat KumarNoch keine Bewertungen
- PPTCT Policy Guideline PDFDokument31 SeitenPPTCT Policy Guideline PDFPabhat KumarNoch keine Bewertungen
- TataNeuApp 1MG 1701053400200Dokument1 SeiteTataNeuApp 1MG 1701053400200Pabhat KumarNoch keine Bewertungen
- 2G CervicalCancer Garbi FINAL VOTINGDokument19 Seiten2G CervicalCancer Garbi FINAL VOTINGAndrea Isabel U. O'DellNoch keine Bewertungen
- Dyadic Approach PDFDokument7 SeitenDyadic Approach PDFPabhat KumarNoch keine Bewertungen
- Birth InjuriesDokument103 SeitenBirth InjuriesAruna ApNoch keine Bewertungen
- Cephalo Pelvic DisproportionDokument43 SeitenCephalo Pelvic DisproportionPabhat KumarNoch keine Bewertungen
- Surgical MenopauseDokument12 SeitenSurgical MenopausePabhat Kumar100% (1)
- KMCPPT 170927065907 PDFDokument30 SeitenKMCPPT 170927065907 PDFPabhat KumarNoch keine Bewertungen
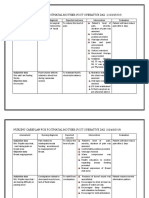
- Nursing Care Plan Assessment Nursing Diagnosis Nursing Goal Nursing Intervention Rationale Outcome Criteria Actual EvaluationDokument4 SeitenNursing Care Plan Assessment Nursing Diagnosis Nursing Goal Nursing Intervention Rationale Outcome Criteria Actual EvaluationPabhat Kumar50% (2)
- Cephalo Pelvic DisproportionDokument43 SeitenCephalo Pelvic DisproportionPabhat KumarNoch keine Bewertungen
- Antenatal Care & ManagementDokument22 SeitenAntenatal Care & ManagementPabhat Kumar100% (3)
- Maxims Hand Out 2Dokument1 SeiteMaxims Hand Out 2Pabhat KumarNoch keine Bewertungen
- Case Study..Care PlanDokument6 SeitenCase Study..Care PlanPabhat Kumar0% (1)
- Case Study..Care PlanDokument6 SeitenCase Study..Care PlanPabhat Kumar0% (1)
- Antenatal Care & Management NewDokument21 SeitenAntenatal Care & Management NewPabhat Kumar100% (3)
- NURSING STANDARDSDokument16 SeitenNURSING STANDARDSPabhat KumarNoch keine Bewertungen
- Skeletal Plan ON National Health Program Related To Child HealthDokument3 SeitenSkeletal Plan ON National Health Program Related To Child HealthPabhat KumarNoch keine Bewertungen
- Parse TheoryDokument33 SeitenParse TheoryPabhat Kumar100% (2)
- Introduction - :: 1. Pre Embryonic PeriodDokument11 SeitenIntroduction - :: 1. Pre Embryonic PeriodPabhat Kumar100% (1)
- ANTENATAL CARE GUIDEDokument23 SeitenANTENATAL CARE GUIDEPabhat Kumar100% (3)
- Case Presentation On Pre-EclampsiaDokument18 SeitenCase Presentation On Pre-EclampsiaPabhat Kumar86% (7)
- Questionnaire: Questionarrie Part-A Code NumberDokument5 SeitenQuestionnaire: Questionarrie Part-A Code NumberPabhat KumarNoch keine Bewertungen
- AntenatalDokument5 SeitenAntenatalPabhat KumarNoch keine Bewertungen
- Antenatal Care & Management NewDokument21 SeitenAntenatal Care & Management NewPabhat Kumar100% (3)
- AntenatalDokument5 SeitenAntenatalPabhat KumarNoch keine Bewertungen
- Report on NRSICON 2018 ConferenceDokument5 SeitenReport on NRSICON 2018 ConferencePabhat KumarNoch keine Bewertungen
- ABSTRACT ItismitaDokument4 SeitenABSTRACT ItismitaPabhat KumarNoch keine Bewertungen
- 7-A Report On AnpDokument10 Seiten7-A Report On AnpPabhat KumarNoch keine Bewertungen
- Ninoy Aquino Parks and Wildlife CenterDokument7 SeitenNinoy Aquino Parks and Wildlife CenterNinia Richelle Angela AgaNoch keine Bewertungen
- Personality Types and Character TraitsDokument5 SeitenPersonality Types and Character TraitspensleepeNoch keine Bewertungen
- 19 - Speed, Velocity and Acceleration (Answers)Dokument4 Seiten19 - Speed, Velocity and Acceleration (Answers)keyur.gala100% (1)
- Gene Regulation: Made By: Diana Alhazzaa Massah AlhazzaaDokument17 SeitenGene Regulation: Made By: Diana Alhazzaa Massah AlhazzaaAmora HZzNoch keine Bewertungen
- Radar PPNDokument5 SeitenRadar PPNSawaf MfNoch keine Bewertungen
- GE - Oil Sheen Detection, An Alternative To On-Line PPM AnalyzersDokument2 SeitenGE - Oil Sheen Detection, An Alternative To On-Line PPM AnalyzersjorgegppNoch keine Bewertungen
- Strategic Management Plan analyzing Unilever's macro and micro environmentsDokument17 SeitenStrategic Management Plan analyzing Unilever's macro and micro environmentsMd Moshiul HaqueNoch keine Bewertungen
- News Writing April 2019Dokument39 SeitenNews Writing April 2019Primrose EmeryNoch keine Bewertungen
- Wirkungen FlechtenstoffeDokument21 SeitenWirkungen FlechtenstoffeLogge UliNoch keine Bewertungen
- Treasure Island Summary c#1-7Dokument4 SeitenTreasure Island Summary c#1-7Great Wall Of FactsNoch keine Bewertungen
- ABB 3HAC050988 AM Arc and Arc Sensor RW 6-En PDFDokument238 SeitenABB 3HAC050988 AM Arc and Arc Sensor RW 6-En PDForefat1Noch keine Bewertungen
- Datasheet Optris XI 410Dokument2 SeitenDatasheet Optris XI 410davidaldamaNoch keine Bewertungen
- My Medications ListDokument5 SeitenMy Medications Listhussain077Noch keine Bewertungen
- AOAC 2012.11 Vitamin DDokument3 SeitenAOAC 2012.11 Vitamin DPankaj BudhlakotiNoch keine Bewertungen
- L C R Circuit Series and Parallel1Dokument6 SeitenL C R Circuit Series and Parallel1krishcvrNoch keine Bewertungen
- Termites and Microbial Biological Control StrategiesDokument30 SeitenTermites and Microbial Biological Control StrategiesMuhammad QasimNoch keine Bewertungen
- Cars Ger Eu PCDokument157 SeitenCars Ger Eu PCsergeyNoch keine Bewertungen
- SDE1 V1 G2 H18 L P2 M8 - SpecificationsDokument1 SeiteSDE1 V1 G2 H18 L P2 M8 - SpecificationsCleverson SoaresNoch keine Bewertungen
- CBSE Worksheet-01 Class - VI Science (The Living Organisms and Their Surroundings)Dokument3 SeitenCBSE Worksheet-01 Class - VI Science (The Living Organisms and Their Surroundings)Ushma PunatarNoch keine Bewertungen
- P3 Past Papers Model AnswersDokument211 SeitenP3 Past Papers Model AnswersEyad UsamaNoch keine Bewertungen
- 841 Specific GravityDokument1 Seite841 Specific GravityJam SkyNoch keine Bewertungen
- Etoh Membrane Seperation I&ec - 49-p12067 - 2010 - HuangDokument7 SeitenEtoh Membrane Seperation I&ec - 49-p12067 - 2010 - HuangHITESHNoch keine Bewertungen
- CLIC Catalogue PDFDokument28 SeitenCLIC Catalogue PDFsangram patilNoch keine Bewertungen
- Advanced Composite Materials Design EngineeringDokument19 SeitenAdvanced Composite Materials Design EngineeringpanyamnrNoch keine Bewertungen
- LIST Real Estate Contacts ListDokument4 SeitenLIST Real Estate Contacts ListChauhan Harshit100% (1)
- 5s OfficeDokument10 Seiten5s OfficeTechie InblueNoch keine Bewertungen
- Kerala Electricity Regulatory Commission Schedule of TariffDokument36 SeitenKerala Electricity Regulatory Commission Schedule of TariffvjtheeeNoch keine Bewertungen
- Frobenius Method for Solving Differential EquationsDokument9 SeitenFrobenius Method for Solving Differential EquationsMario PetričevićNoch keine Bewertungen
- Edexcel A-Level Biology Experimental Design Marks Scheme (1) (Full Permission)Dokument16 SeitenEdexcel A-Level Biology Experimental Design Marks Scheme (1) (Full Permission)FardeenKhanNoch keine Bewertungen
- ADDC Construction QuestionairesDokument19 SeitenADDC Construction QuestionairesUsman Arif100% (1)