Beruflich Dokumente
Kultur Dokumente
Criza Convulsiva 2
Hochgeladen von
ralucast880 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
9 Ansichten45 SeitenAlgoritm urgenta
Originaltitel
12.-Criza-convulsiva-2
Copyright
© © All Rights Reserved
Verfügbare Formate
PPTX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenAlgoritm urgenta
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
9 Ansichten45 SeitenCriza Convulsiva 2
Hochgeladen von
ralucast88Algoritm urgenta
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 45
Carrie de Moor, MD
Associate Medical Director/ED Trauma Director
JPS Health Network
4/21/2012
Recognize potential difficult airways
Review Techniques for Advanced Airway
Management
Understand options for sedation in RSI during
a national shortage of Etomidate
Become familiar with new advanced airway
management tools
Poor oxygenation or ventilation
Inability to protect the aiway (Decreased
LOC/GCS, secretions, swelling, severe facial
trauma)
Potential for rapid deterioration
Patient/Staff safety ( The acutely agitated
patient)
Positioning
Assistance at bedside (nursing/RT)
Time to prepare and plan
Fasting patient
Ability to abort the procedure
Anesthesia/surgical back up available
Intact, clear airway
Wide open mouth
Pre-Oxygenated
Intact respiratory drive
Normal dentition
Normal and Easily identifiable anatomy
Good Neck Mobility
This ideally should occur before you attempt!
Review Past Medical History
Physical Exam
Mallampati Classification
Thyromental Distance
Obvious deformities/Trauma
Signs of obstruction
Neck Mobility
Previous Difficult Intubations
Previous Surgical Airway
Congenital Conditions- Pierre Robin Syndrome
Arthritis- Rheumatoid, Ankylosing Spondylitis
Prior C-spine/Neck Surgeries
Head and Neck tumors
Limited Neck Mobility
Facial Instability
Burns
Obesity or very small.
Short Muscular neck
Receding Jaw
Signs of Anaphylaxis
Stridor/FBAO
Scars from Previous Surgeries
Is there blood in the airway?
Is the patient actively vomiting?
Are there teeth missing?
Is there clinical suspicion for Epiglottitis, RPA,
or Ludwig’s Angina?
Is the patient immobilized?
Consider Alternatives for Airway Support
CPAP/BiPAP
Call Backup/Intubation in controlled OR setting
Prepare for need to change equipment
Different blades
Different tube sizes
Bougie
LMA/Combitube
Advanced Airway Equipment- Glidescope, Fiberoptics
etc
Prepare for Surgical Airway
Sellick’s Maneuver/Cricoid Pressure ( +/-)
BURP maneuver
Good Positioning- Sniff position
Always have a bougie in your pocket
Cricothyrotomy
• Application of pressure to a patient’s cricoid cartilage during
endotracheal intubation to prevent aspiration
• Pitfalls:
• Potential for Airway obstruction
• Evidence that it actually prevents aspiration is lacking
• A 2007 study published in Annals of Emergency Medicine
recommended that “the removal of cricoid pressure be an
immediate consideration if there is any difficulty either in
intubating or ventilating the ED patient.” (Ellis)
BURP : “backward-upward-rightward
pressure” of the larynx
Displaces the thyroid cartilage dorsally so that the
larynx is pressed against cervical vertebrae’s body
Ideally two centimeters in cephalic direction, until
resistance is felt
Next it should be displaced 0.5 cm -2.0 cm rightward
When used with Sellick’s may actually worsen
view
Sniffing Position
First Described in 1936 by Bannister and MacBeth- to
align oral, pharyngeal, laryngeal axes to provide
optimal exposure of the glottis
Pitfalls: Inadequate for the morbidly obese
patient, not an option with suspected cervical
spine injury
Ear-to-sternal notch positioning improves the
mechanics of ventilation, both with
spontaneous breathing, and with mask
ventilation.
In the obese patient: shoulders are elevated, the
head and neck are extended, and the external
auditory meatus is in line with the sternal
notch
Figure 1. Elevated head-up position.
Zvara D A et al. Anesth Analg 2006;102:1592-1592
©2006 by Lippincott Williams & Wilkins
Figure 2. Whelan-Calicott position.
Zvara D A et al. Anesth Analg 2006;102:1592-1592
©2006 by Lippincott Williams & Wilkins
Atlanto-occipital extension is necessary to
bring the vocal cords within line-of-sight of the
mouth, manual axial in-line stabilization
reduces this movement by 60%.
Bougie for Intubation
Video
“Hey Doc.. We’re out of Etomidate”
There are a number of options for RSI- choose
wisely
Succinylcholine vs. Rocuronium/Vecuronium
Consider potential for awake
intubation/sedated but not paralyzed
intubation
Know your drugs and your doses
Dosage: 2-3 mg/kg IV Push
Onset of action: < 1 minute
Duration 3-10minutes
Benefits: Rapid onset, brief duration, amnestic
Caution: Causes cardiovascular depression and
hypotension
Dosage: 1-2mg/kg slow IVP
Onset: 30 seconds to 1 minute
Duration: 5-10 minutes
Benefits: Potent Bronchodilator, leaves
protective airway reflexes intact, maintains
cardiovascular stability
Caution: Old Dogma regarding elevated ICP
with use, increases sympathetic tone,
emergence delirium common
Often underutilized due to old dogma regarding
ICP
Ketamine is a non-competitive NMDA receptor
antagonist and has neuroprotective effects
Studies claiming ketamine should be avoided in
head injury are based on 3 studies from the 1970’s,
recent studies have shown no convincing evidence
that these claims are valid
Acute agitation and emergence reactions may be of
concern for conscious sedation. However, in the
RSI population where continued sedation with
benzodiazepines is possible, this is of less concern.
Dosage needs vary from patient to patient
Onset of action can be unpredictable
Poor choice for true Rapid Sequence Intubation
Cost: $11,000 for the Cobalt
Benefits: Easy to use, easy to observe
student/resident procedures, minimal need to
manipulate the neck
Features- Pediatric and Adult Sizes, unique 60
degree blade, disposable and reusable options
3 options: Cobalt, Ranger, GVL
Pitfalls: Expensive, limited visibility with
significant secretions or blood
Cost: $700-800
Benefits: Easily portable, affordable, no need
for special stylette
Pitfalls: Lower resolution than glidescope, less
useful in teaching scenarios due to size of
screen
Cost: $60,000
Benefits: Maintains the same curvature are the
basic MAC blade, may be used for
conventional direct laryngoscopy or with video
assistance, benefits for teaching scenarios
Pitfalls: Price, mobility
Abrams K.J., Grande C.M. "Airway Management of the trauma patient with cervical spine
injury", Current Opinion in Anesthesiology 1994;7:184-190
The BURP Maneuver . Images in Anesthesiology .Vol. 31. No. 1 January-March 2008 pp
63-6
Cattano, D. Cavallone, L. Airway Management and Airway Positioning: A Clinical
Perspective. Anesthesiology News. 2010:35-40.
Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid
sequence tracheal intubations: A risk-benefit analysis. Annals of Emergency
Medicine. 2007;50:653-665
EmCrit. “Use of the Bougie for Intubation” http://youtu.be/E7Lo1JD2Brk
Hastings R.H., Marks J.D. "Airway Management for Trauma Patients with Potential Cervical
Injuries", Anesth Analg 1991;73:471-82.
Zvara D A et al. Positioning for Intubation in Morbidly Obese Patients Anesth Analg
2006;102:1592-1592
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Manage Odontogenic Infections Stages Severity AntibioticsDokument50 SeitenManage Odontogenic Infections Stages Severity AntibioticsBunga Erlita RosaliaNoch keine Bewertungen
- Acne and Whey Protein Supplementation Among Bodybuilders PDFDokument4 SeitenAcne and Whey Protein Supplementation Among Bodybuilders PDFHenyta TsuNoch keine Bewertungen
- Embryology GenitalDokument53 SeitenEmbryology GenitalDhonat Flash100% (1)
- Cerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluidDokument5 SeitenCerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluiderickNoch keine Bewertungen
- S0300 9572 (15) 00330 5 - MainDokument21 SeitenS0300 9572 (15) 00330 5 - MainxxnetNoch keine Bewertungen
- Guias Europeas RCCPDokument19 SeitenGuias Europeas RCCPDiana MontesNoch keine Bewertungen
- S0300 9572 (15) 00342 1 - MainDokument14 SeitenS0300 9572 (15) 00342 1 - MainxxnetNoch keine Bewertungen
- Trauma GravidaDokument39 SeitenTrauma Gravidaralucast88Noch keine Bewertungen
- S0300 9572 (15) 00341 X - MainDokument15 SeitenS0300 9572 (15) 00341 X - MainxxnetNoch keine Bewertungen
- S0300 9572 (15) 00329 9 - MainDokument54 SeitenS0300 9572 (15) 00329 9 - MaintugurlanNoch keine Bewertungen
- S0300 9572 (15) 00341 X - MainDokument15 SeitenS0300 9572 (15) 00341 X - MainxxnetNoch keine Bewertungen
- S0300 9572 (15) 00330 5 - MainDokument21 SeitenS0300 9572 (15) 00330 5 - MainxxnetNoch keine Bewertungen
- Meningitis Pediatrics in Review Dic 2015Dokument15 SeitenMeningitis Pediatrics in Review Dic 2015Edwin VargasNoch keine Bewertungen
- Drug Control Policy of BangladeshDokument51 SeitenDrug Control Policy of BangladeshHedayat Ullah33% (3)
- Rangkuman by Yulia VionitaDokument21 SeitenRangkuman by Yulia VionitaRizqi AkbarNoch keine Bewertungen
- MYMAN Chanchinbu Issue No. 5Dokument6 SeitenMYMAN Chanchinbu Issue No. 5Langa1971Noch keine Bewertungen
- Pedigree Analysis: (Cf. Chapters 4.4, 5.2, 6.2 of Textbook)Dokument11 SeitenPedigree Analysis: (Cf. Chapters 4.4, 5.2, 6.2 of Textbook)Kristyne OliciaNoch keine Bewertungen
- HPLC - 4Dokument24 SeitenHPLC - 4Melisa Soledad Barco Jara100% (1)
- Chapter 6 DiscussionDokument3 SeitenChapter 6 DiscussionyughaNoch keine Bewertungen
- Class III Cavity Treatment (Procedure, Materials)Dokument2 SeitenClass III Cavity Treatment (Procedure, Materials)Manos KritikosNoch keine Bewertungen
- 4 Levels of Perio DZDokument2 Seiten4 Levels of Perio DZKIH 20162017Noch keine Bewertungen
- Pediatric PerfectionismDokument20 SeitenPediatric Perfectionismapi-438212931Noch keine Bewertungen
- Resume Massage Therapist NtewDokument2 SeitenResume Massage Therapist NtewPartheebanNoch keine Bewertungen
- Effects of Pulmonary Rehabilitation On Physiologic and Psychosocial Outcomes in Patients With Chronic Obstructive Pulmonary DiseaseDokument10 SeitenEffects of Pulmonary Rehabilitation On Physiologic and Psychosocial Outcomes in Patients With Chronic Obstructive Pulmonary DiseaseElita Urrutia CarrilloNoch keine Bewertungen
- Presentation - Oral Controlled Release DrugDokument38 SeitenPresentation - Oral Controlled Release DrugMrValentynNoch keine Bewertungen
- LSM RepairDokument4 SeitenLSM RepairDanily Faith VillarNoch keine Bewertungen
- Vaginitis: Diagnosis and TreatmentDokument9 SeitenVaginitis: Diagnosis and TreatmentAbigail MargarethaNoch keine Bewertungen
- Critical Perspectives - Dissertation OgrDokument15 SeitenCritical Perspectives - Dissertation OgrPipNoch keine Bewertungen
- Lecture 16-17 - Opioids AnalgesicsDokument20 SeitenLecture 16-17 - Opioids AnalgesicsJedoNoch keine Bewertungen
- Maxillofacial Privileges QGHDokument4 SeitenMaxillofacial Privileges QGHSanam FaheemNoch keine Bewertungen
- A Client With A Brain Tumor: Nursing Care PlanDokument1 SeiteA Client With A Brain Tumor: Nursing Care Planshabatat2002Noch keine Bewertungen
- Mental Health Personal Statement - Docx'Dokument2 SeitenMental Health Personal Statement - Docx'delson2206Noch keine Bewertungen
- Sepsis Content Concepts MapDokument2 SeitenSepsis Content Concepts Mapghodghod1230% (1)
- Canadian Standards For Hospital LibrariesDokument4 SeitenCanadian Standards For Hospital LibrariesFernando HernandezNoch keine Bewertungen
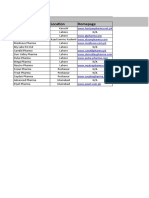
- End users' contact and product informationDokument3 SeitenEnd users' contact and product informationمحمد ہاشمNoch keine Bewertungen
- Week - 4 - H2S (Hydrogen Sulfide) Facts W-Exposure LimitsDokument2 SeitenWeek - 4 - H2S (Hydrogen Sulfide) Facts W-Exposure LimitsLọc Hóa DầuNoch keine Bewertungen
- Daftar Regulasi Bidang KeperawatanDokument128 SeitenDaftar Regulasi Bidang KeperawatanSanti AndrianiNoch keine Bewertungen