Beruflich Dokumente
Kultur Dokumente
Mitigation Response To Influenza A (H1N1) - v2
Hochgeladen von
gem_jae020 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
9 Ansichten24 SeitenOriginaltitel
Mitigation Response to Influenza A (H1N1)_v2
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
9 Ansichten24 SeitenMitigation Response To Influenza A (H1N1) - v2
Hochgeladen von
gem_jae02Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 24
Mitigation Response to Influenza
A (H1N1) Virus Infection
National Center for Disease Prevention and Control, DOH
Objectives
• To slow down the virus spread in the
community & minimize transmission to the
most vulnerable group
• To improve health facility preparedness in
providing necessary treatment particularly for
severe cases to reduce mortality impact
• To minimize social disruption & other negative
consequences
National Center for Disease Prevention and Control, DOH
Severity Assessment
• Virological factor (Properties of the virus)
– Self-limiting infections in majority of infected
individuals
– Can cause very sever form of infections among the
high risk group
• Population vulnerability
– Relatively high in the Philippines
• Capacity to respond
– Established outbreak response mechanism at national
& regional levels
National Center for Disease Prevention and Control, DOH
Components/Framework of Response
• Command system
• Surveillance
• Health facility response
• Public health interventions
• Risk communication
National Center for Disease Prevention and Control, DOH
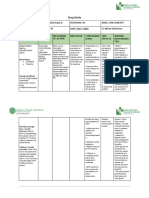
Stepwise Approach
• Mitigation response level 1
– A few sporadic cases
– No clustering of cases
– No community level transmission
• Mitigation response level 2
– Beginning of community level transmission
– Clustering of confirmed cases of Influenza A (H1N1) in defined
communities or specific areas (schools, workplace, etc...)
• Mitigation response level 3
– Sustained community transmission
– A series of clusters in a population in a given period of time &
becoming wider in a given geographical area
National Center for Disease Prevention and Control, DOH
Response Matrix
Command System
• DOH Task Force (National / CHDs)
• NDCC / RDCC (DOH Secretary is the de facto chair currently)
• Local Task Force on Influenza A (H1N1)
• Provincial, municipal, city
Command system should be functional at all mitigation response levels
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 1
Surveillance Health Facility Response
•Laboratory Surveillance •Identify referral hospitals
• If it fits the case definition of Case Under • check number of beds, isolation rooms,
Observation, needs to perform respirators, etc...
confirmatory exam • Capacitate referral hospitals to manage
• Disease Surveillance confirmed cases
• Look for clustering of cases • Intensify infection control
• If with clustering of ILI, needs to • Prepare essential meds & equipments incl.
perform random confirmatory exam protocols
• Contact tracing • Admit ALL confirmed cases
• Event based surveillance • Antiviral meds to all probable & confirmed
cases
• Prepare RHU / Health Centers / Private clinics
& Primary hospitals to manage mild cases,
ambulatory cases or screen ILI & establish
referral system for severe cases
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 1
Public Health Interventions Risk Communication
•Containment measures • Focus on individual, household & public
• Non-pharmaceutical interventions awareness
• Quarantine • Prevention
• Isolation • Infection control
• Social distancing • Hand hygiene
• School closure • Cough manners
• intensify infection control program in the • Containment
community • Provide accurate & up to date information
• infection control committee, trainings, • Prepare, reproduce & distribute information
available PPEs, protocols materials specific for containment & mitigation
measures
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 2
Surveillance Health Facility Response
•Laboratory Surveillance •If community transmission has been observed in
• If it fits the case definition of CUO, needs the affected area:
to perform confirmatory exam • Mild cases to be observed / managed at
• Scale up lab capacity to cope up with the home
increasing number of CUO • Admit probable & confirmed cases
• When community transmission has been showing signs of respiratory infections &
established in an area, conduct random severe medical conditions
sampling of CUOs to establish if there is •Treatment dose of Oseltamivir for the
sustained transmission compromised / vulnerable sick group
• Disease Surveillance • No prophylaxis dose for close contacts
• Establish the extent of spread of the except for health care providers exposed to
disease & if there is sustained community probable & confirmed case without use of
level transmission appropriate PPE
• Event based surveillance • Triaging at the hospitals, public health
• If community transmission has been centers & clinics
established, no need to perform contact • Hospitals, health centers & clinics should be
tracing ready to handle surge of consultations & possible
admissions or referrals
• Intensify infection control in hospitals, health
centers & clinics
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 2
Public Health Interventions Risk Communication
•Non-pharmaceutical interventions • Focus on individual, household & public
• Home confinement / Isolation of mild cases awareness
• Isolation for cases admitted in hospitals • Prevention
• Social distancing for close contacts • Infection control same as level 1
• Social distancing like school closure will • Containment
depend on local epidemiological situation • Mitigation measures
• intensify infection control program in the • Provide accurate & up to date information
community • Special attention to the vulnerable group of
• infection control committee, trainings, available population most likely to develop complications
PPEs, protocols • Emphasize self quarantine for the exposed &
home treatment for the mild cases, early
consultation to prevent complications & severe
outcome of the disease
• Continuous information to the public through IEC
• Communication should focus on the DOH best
efforts to contain the disease, until such time that
mitigation process has to start
• Mitigation process has to be proactive
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 3
Surveillance Health Facility Response
•Laboratory Surveillance •Admit severe respiratory infections & with
• RITM & other laboratory to prioritize severe medical conditions
high risk groups • Public & private hospitals should be prepared
•Lab exam to include monitoring the to manage higher number of complicated,
properties of the virus (mutation, severe cases
resistance, etc...) •Health centers, RHUs / private clinics should
• Disease Surveillance be prepared to manage higher number of mild
• No more contact tracing cases as out patient or ambulatory cases
• Monitoring disease to know if activity • Prioritize treatment dose of oseltamivir
levels are going up or down •Public health facilities (RHUs, health centers)
• Monitor changes in the natural history to be ready to admit severe / complicated
of the disease cases once the surge capacity of the hospitals
can no longer address the need of the
pandemic
National Center for Disease Prevention and Control, DOH
Mitigation Response Level 3
Public Health Interventions Risk Communication
•Non-pharmaceutical interventions same as • Sustain level of public awareness
above • Mitigation measures
• Use of appropriate PPEs, facility modified to • Infection control
cater the infection control measure needs, • Provide accurate & up to date information
systems flow • Minimize fear, anxiety & unrest
• Debriefing of frontline health workers • Continuous information to the public through
IEC
• Referral system must be functional in all mitigation response levels
National Center for Disease Prevention and Control, DOH
Major Policy Changes from
Containment to Mitigation Response
to the Influenza A (H1N1) Outbreak in
the Country
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
Infection Control Measures Provisions of Interim In response to observation of
Guidelines Nos. 1 to 15 (issued index cases & cohort of cases
between May 4 to June 8, & WHO Pandemic Phase 6
2009)
1. Prophylaxis with the anti- • For ALL first responders or SELECTIVE Prophylaxis
viral (oseltamivir) health care workers tending • Post exposure prophylaxis
suspected, probable & ONLY for close contacts with
confirmed cases existing unstable medical
• For ALL household & close conditions that may be
contacts aggravated by a viral infection
(Interim Guidelines nos. 1, 2 & • NO pre-exposure prophylaxis
8) for health care workers or first
responders
• Post exposure prophylaxis for
health care workers who did
not have adequate PPE when
in contact with confirmed
cases
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
2. Anti-viral treatment for • For ALL confirmed (positive) Limited to specific indications
confirmed Influenza A (H1N1) cases of Influenza A (H1N1) & with medical supervision
cases (Interim Guidelines nos. 1 & 2) • Anti-viral treatment ONLY for
confirmed cases with:
• Severe or progressive
illness
• Pre-existing or
concurrent medical
condition that
compromise system or
pulmonary function
• Emphasize: Use anti-viral in
pregnancy ONLY when
benefits outweigh the risk to
embryo or fetus
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
3. Quarantine Rule for • Home quarantine for 10 days RESPONSIBLE SELF
Travellers for ALL travellers coming from MONITORING
countries reporting confirmed • Travellers shall monitor self
cases of Influenza A (H1N1), for 10 days after arrival,
with or without ILI observe for signs & symptoms
of ILI & submit to National
DOH Guidelines if ILI develops
• For patients diagnosed as
confirmed case of Influenza A
(H1N1) & intending to travel
outside the Philippines, travel
clearance shall be provided 7
days after resolution of fever
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
4. Confinement or isolation & • For ALL suspected cases or RESPONSIBLE, VOLUNTARY
quarantine measures for CUO (ILI & history of recent CONFINEMENT
suspected cases or CUOs travel or exposure to • In general, voluntary home
confirmed cases) until confinement
laboratory results are obtained • Hospital admission only
(Interim Guidelines no. 15) when clinically indicated
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
5. Confinement or Isolation of • “Probable & confirmed cases MEDICALLY PRESCRIBED
Probable or Confirmed Cases shall remain in confinement... Hospital Confinement
until asymptomatic” • A great majority of probable
(Interim Guidelines no. 2) & confirmed cases are for
home care. They are those
with stable clinical
manifestations or those
identified when they were in
the recovery stage of the
illness
• Hospital admission criteria
include those manifesting with
respiratory difficulty,
progressively acute illness &
debility & others belonging to
risk groups
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
6. Laboratory Diagnosis • For suspected cases & CUOs SELECTIVE Laboratory
•At the Research Institute for Confirmatory Testing
Tropical Medicine • Indications for laboratory testing
(Interim Guidelines nos. 3, 7 & 15) are:
• Mandatory investigation of
CUOs identified at various
ports of entry in the country
• Investigation of first
suspect cases in a specific
area or community
• Random sampling of
persons in clusters with ILI
manifesting with unusual
symptoms or severity
• Investigation of ILI in
persons at high risk of
developing complications
because of other medical
conditions or problems
• NO LABORATORY FOLLOW-UP
TESTS ARE NECESSARY PRIOR TO
DISCHARGE
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
7. Reporting of Influenza A • Mandatory reporting of ILI • Routine reporting of ILI
(H1N1) Suspects or CUOs among travellers from through the nationwide
countries where there are Philippine Integrated Disease
confirmed cases & of close & Surveillance Reporting
contacts of confirmed cases System (PIDSR)
• Reporting of all rumors on • Pursue screening & reporting
occurence of ILIs of persons with ILI detected at
(Interim Guidelines no. 7) international ports of entry
National Center for Disease Prevention and Control, DOH
Major Policy Changes
FROM TO
8. Contact Tracing • For ALL close contacts of • Routine contact tracing for
confirmed cases disease investigation shall only
(Interim Guidelines no. 14) be conducted to document
first & second generation
transmission in communities
or specific areas with no
previous cases based on the
assessment of CHDs & local
health officials
National Center for Disease Prevention and Control, DOH
Individuals at Increased Risk for
Hospitalizations and Death
• Elderly > 60 years
• Children less than two years
• Certain chronic diseases
– Heart or lung disease, including asthma, pneumonia who needs
hospitalization in 2nd or 3rd level of care
– Metabolic disease, including uncontrolled diabetes
– HIV/AIDs, other immunosuppression, organ transplant patient
– Conditions that can compromise respiratory function or the handling
of respiratory secretions like COPD, PTB (active & untreated), MDRTB
or previous pulmonary pathology which requires hospitalization
– Patient with rapid progression of disease
– Patient with criterion for admission in ICU
– Patient with severe malnutrition
National Center for Disease Prevention and Control, DOH
Individuals at Increased Risk for
Hospitalizations and Death
• Certain chronic diseases
– Complex congenital cardiopathy that requires hospitalization in 2nd or
3rd level of care
– Chronic renal insufficiency that requires hospitalizations
– Heart defect or previous cardiac pathology that requires
hospitalization
– Patients with underlying chronic diseases that present progression to
deterioration
• Pregnant women
National Center for Disease Prevention and Control, DOH
Thank You!
National Center for Disease Prevention and Control, DOH
Das könnte Ihnen auch gefallen
- Control of Communicable DiseasesDokument38 SeitenControl of Communicable Diseasesvoruganty_vvs100% (1)
- Chapter 7outbreak InvesDokument25 SeitenChapter 7outbreak InvesEstiv W. StigNoch keine Bewertungen
- Topic 3 - Disease Control StrategiesDokument25 SeitenTopic 3 - Disease Control StrategiesKaey NiezamNoch keine Bewertungen
- Communicable Diseases GuideDokument44 SeitenCommunicable Diseases GuidexilcomNoch keine Bewertungen
- Managing COVID-19 Cases in the CommunityDokument18 SeitenManaging COVID-19 Cases in the CommunityElteyb Nor eldaimNoch keine Bewertungen
- Guidance On Contact Tracing For: COVID-19 PandemicDokument16 SeitenGuidance On Contact Tracing For: COVID-19 PandemicSOFIA CATALINA CORTES VELASQUEZ100% (1)
- WHO Information Network For Epidemics: WWW - Who.int/epi-WinDokument5 SeitenWHO Information Network For Epidemics: WWW - Who.int/epi-WinKannan JaganNoch keine Bewertungen
- Cme On TuberclosisDokument12 SeitenCme On TuberclosisOdulusi DanielNoch keine Bewertungen
- Servillance and Out BreakDokument79 SeitenServillance and Out BreakruthNoch keine Bewertungen
- Final Info KitDokument42 SeitenFinal Info KitDolly BenitezNoch keine Bewertungen
- Principles Contact Tracing BookletDokument3 SeitenPrinciples Contact Tracing Bookletjoeboots78Noch keine Bewertungen
- Chapter 5 Public HealthDokument36 SeitenChapter 5 Public HealthNUR ' AMIRAH BINTI ABDUL GHAFAR / UPMNoch keine Bewertungen
- Health Information Systems GuideDokument25 SeitenHealth Information Systems Guideflordeliza magallanesNoch keine Bewertungen
- Role of Primary Care in The COVID-19 Response: Interim GuidanceDokument8 SeitenRole of Primary Care in The COVID-19 Response: Interim GuidanceGabriellaNoch keine Bewertungen
- Dengue FeverDokument1 SeiteDengue Feverapi-266482250Noch keine Bewertungen
- National Dengue Prevention ProgramDokument26 SeitenNational Dengue Prevention ProgramFranz Anthony Quirit GoNoch keine Bewertungen
- National Dengue Prevention and Control ProgramDokument26 SeitenNational Dengue Prevention and Control ProgramFranz Anthony Quirit GoNoch keine Bewertungen
- Group 1 InfographicsDokument2 SeitenGroup 1 Infographicscabahugjabez192Noch keine Bewertungen
- Nosocomial InfectionDokument29 SeitenNosocomial InfectionNikhil DeurkarNoch keine Bewertungen
- Acute Haemorrhagic Fever Syndrome: Rationale For SurveillanceDokument17 SeitenAcute Haemorrhagic Fever Syndrome: Rationale For SurveillanceKabiralYusufPriyonoNoch keine Bewertungen
- Lessons From Wuhan COVID 19 03 12 2020 - RevisedDokument51 SeitenLessons From Wuhan COVID 19 03 12 2020 - RevisedZishanNoch keine Bewertungen
- Module 1 Identify and Record Cases of Priority Diseases, Conditions or Events - 7augDokument49 SeitenModule 1 Identify and Record Cases of Priority Diseases, Conditions or Events - 7augSolomon Fallah Foa SandyNoch keine Bewertungen
- 48862-Article Text-64398-1-10-20091209Dokument3 Seiten48862-Article Text-64398-1-10-20091209raja yasminNoch keine Bewertungen
- NCM110 Nursing Informatics FinalsDokument7 SeitenNCM110 Nursing Informatics FinalsSteph CaronanNoch keine Bewertungen
- Session 9 Presentation Managing C19 in Nursing HomesDokument20 SeitenSession 9 Presentation Managing C19 in Nursing Homesleena elizabethNoch keine Bewertungen
- Guidelines For Investigation and Management ofDokument25 SeitenGuidelines For Investigation and Management ofronicaNoch keine Bewertungen
- Diagnosis & Evaluation: SmallpoxDokument9 SeitenDiagnosis & Evaluation: SmallpoxPravesh VermaNoch keine Bewertungen
- Outbreak Investigation and Management: Chapter TenDokument74 SeitenOutbreak Investigation and Management: Chapter TenYimesgen YirgaNoch keine Bewertungen
- Principles of Epidemic Outbreak InvestigationDokument46 SeitenPrinciples of Epidemic Outbreak Investigationkuchie ranksNoch keine Bewertungen
- Social Distancing Measures in Response To The COVID 19 EpidemicDokument10 SeitenSocial Distancing Measures in Response To The COVID 19 EpidemicntnquynhproNoch keine Bewertungen
- Issue 76 - March 2012Dokument24 SeitenIssue 76 - March 2012Charles HackettNoch keine Bewertungen
- DOTSLong 5.4Dokument2 SeitenDOTSLong 5.4JAY JR. APONNoch keine Bewertungen
- Umvuzo Health Member Communication On COVID-19Dokument4 SeitenUmvuzo Health Member Communication On COVID-19BenNoch keine Bewertungen
- COVID-19 Update: Community Organizations Active in Disaster (COADDokument20 SeitenCOVID-19 Update: Community Organizations Active in Disaster (COADTom FlesherNoch keine Bewertungen
- Outbreak InvestigationDokument17 SeitenOutbreak InvestigationNathnael GebNoch keine Bewertungen
- Outbreak EpdDokument40 SeitenOutbreak EpdKedir AhmedNoch keine Bewertungen
- Clostridium Difficile Infection (CDI) : Prevention PrimerDokument80 SeitenClostridium Difficile Infection (CDI) : Prevention PrimererpNoch keine Bewertungen
- Tuberculosis Prevention CampaignDokument20 SeitenTuberculosis Prevention CampaignTaranum RandhawaNoch keine Bewertungen
- Communicable Diseases 101Dokument38 SeitenCommunicable Diseases 101Delechos JaysonNoch keine Bewertungen
- Emergency Room NursingDokument12 SeitenEmergency Room Nursingray100% (1)
- Safety of Patients in Pandemic in MedicineDokument20 SeitenSafety of Patients in Pandemic in Medicineovi booksNoch keine Bewertungen
- Diseases of Public Health SignificanceDokument34 SeitenDiseases of Public Health SignificanceMelesNoch keine Bewertungen
- Communicable Diseases 101Dokument38 SeitenCommunicable Diseases 101kunalphalswal0005Noch keine Bewertungen
- Epidemiology and Surveillance OverviewDokument35 SeitenEpidemiology and Surveillance OverviewKay BristolNoch keine Bewertungen
- Week 15 Outbreak InvestigationDokument13 SeitenWeek 15 Outbreak InvestigationAngeline LimNoch keine Bewertungen
- NYC's multifaceted approach to outbreak detectionDokument31 SeitenNYC's multifaceted approach to outbreak detectionf3er3Noch keine Bewertungen
- IPC BasicsDokument31 SeitenIPC BasicsSherwin CruzNoch keine Bewertungen
- NOTES CD Lecture Generic 2022Dokument182 SeitenNOTES CD Lecture Generic 2022Meryville JacildoNoch keine Bewertungen
- National Aids Control ProgDokument45 SeitenNational Aids Control ProgGirishkumar KrishnaNoch keine Bewertungen
- Steps in a Foodborne Outbreak InvestigationDokument22 SeitenSteps in a Foodborne Outbreak InvestigationMaria PavlovaNoch keine Bewertungen
- Prevention of Infection: Infectious Diseases Global HealthDokument12 SeitenPrevention of Infection: Infectious Diseases Global HealthsaravananNoch keine Bewertungen
- Sampling & Field InvestigationDokument23 SeitenSampling & Field InvestigationBashiru GarbaNoch keine Bewertungen
- Iq Panel Training Slides (Final Revisions)Dokument138 SeitenIq Panel Training Slides (Final Revisions)taylorNoch keine Bewertungen
- Sexually Transmitted Disease Control ProgrammeDokument17 SeitenSexually Transmitted Disease Control ProgrammeMilan NayekNoch keine Bewertungen
- Communicable Disease - Askep Penyakit MenularDokument29 SeitenCommunicable Disease - Askep Penyakit MenularPuteri AtigaNoch keine Bewertungen
- WHO 2019 nCoV Cases - Clusters - Investigation 2020.2 Eng PDFDokument4 SeitenWHO 2019 nCoV Cases - Clusters - Investigation 2020.2 Eng PDFرجاء خاطرNoch keine Bewertungen
- Field Investigation For Zoonotic Diseases 29072022Dokument48 SeitenField Investigation For Zoonotic Diseases 29072022Kalpanah GurumurthyNoch keine Bewertungen
- Saint - Lucia COVID-19 Community ManagenentDokument18 SeitenSaint - Lucia COVID-19 Community ManagenentOqba AlzwainyNoch keine Bewertungen
- SafeStartWA 4may20 PDFDokument9 SeitenSafeStartWA 4may20 PDFSergio ImbrigiottaNoch keine Bewertungen
- Jesus' final words from the crossDokument4 SeitenJesus' final words from the crossgem_jae02Noch keine Bewertungen
- Blood Normal ValuesDokument1 SeiteBlood Normal ValuesDoris Glenn FloresNoch keine Bewertungen
- Urinary System DisordersDokument8 SeitenUrinary System Disordersgem_jae02Noch keine Bewertungen
- Report in Trans. Nx.Dokument51 SeitenReport in Trans. Nx.gem_jae02Noch keine Bewertungen
- Drug Study PDFDokument14 SeitenDrug Study PDFsretirado02Noch keine Bewertungen
- (Asking-Reporting Health Problem and Diagnosing)Dokument10 Seiten(Asking-Reporting Health Problem and Diagnosing)nilanNoch keine Bewertungen
- Learners' Activity Sheets: Health 8Dokument11 SeitenLearners' Activity Sheets: Health 8Leode Joy Tulang100% (1)
- Cutaneous Microabscesses by Mycobacterium Chelonae: Case Reports From A Tertiary Care Centre, TripuraDokument4 SeitenCutaneous Microabscesses by Mycobacterium Chelonae: Case Reports From A Tertiary Care Centre, TripuraIJAR JOURNALNoch keine Bewertungen
- About Quinine For MalariaDokument2 SeitenAbout Quinine For MalariaYeewanNgNoch keine Bewertungen
- Medical Examination FormDokument3 SeitenMedical Examination Formchumbefred25% (4)
- Isolation TechniqueDokument19 SeitenIsolation Techniquejenn21283% (6)
- Patient Zero Infectious Prac1Dokument2 SeitenPatient Zero Infectious Prac1api-536437763Noch keine Bewertungen
- Effect Modification, Bias, and Causal Inference in EpidemiologyDokument57 SeitenEffect Modification, Bias, and Causal Inference in EpidemiologygygNoch keine Bewertungen
- Case Study - Nephrotic SyndromeDokument42 SeitenCase Study - Nephrotic Syndromefarmasi rsud cilincingNoch keine Bewertungen
- Normal and Abnormal Characteristic of SputumDokument2 SeitenNormal and Abnormal Characteristic of SputumKim Chamos100% (2)
- Probiotic HandoutDokument2 SeitenProbiotic Handoutapi-243273519Noch keine Bewertungen
- New Diagnostic Test For Dogs With Chronic Gastrointestinal SignsDokument2 SeitenNew Diagnostic Test For Dogs With Chronic Gastrointestinal SignsvetthamilNoch keine Bewertungen
- Tatalaksana Hiperosmolar Hiperglicemic State (SHH)Dokument16 SeitenTatalaksana Hiperosmolar Hiperglicemic State (SHH)Vidya VidyutNoch keine Bewertungen
- Human Parasitic Amoebas: Topic OutlineDokument10 SeitenHuman Parasitic Amoebas: Topic OutlineSam Raven AndresNoch keine Bewertungen
- Prevalence of Helminthes Infection in Stray Dogs in Ilam ProvinceDokument4 SeitenPrevalence of Helminthes Infection in Stray Dogs in Ilam ProvinceRaisis Farah DzakiyyahNoch keine Bewertungen
- c23 Microbiology Tortora TestbankDokument16 Seitenc23 Microbiology Tortora Testbankwhitewave25Noch keine Bewertungen
- Ref. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Dokument2 SeitenRef. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Bhagat DeepakNoch keine Bewertungen
- Phytochemicals Health Promotion and Therapeutic Potential (PDFDrive) PDFDokument264 SeitenPhytochemicals Health Promotion and Therapeutic Potential (PDFDrive) PDFPaulo Aguiar100% (1)
- Infectious DiseasesDokument6 SeitenInfectious DiseasesAlexa QuizomNoch keine Bewertungen
- Dr. HY Peds Shelf Parts 1 & 2Dokument22 SeitenDr. HY Peds Shelf Parts 1 & 2Emanuella GomezNoch keine Bewertungen
- IntroductionDokument1 SeiteIntroductionLuna JadeNoch keine Bewertungen
- BLA CK DEA TH: Spanis H FluDokument24 SeitenBLA CK DEA TH: Spanis H FluShiela FranciscoNoch keine Bewertungen
- ConjuntivitisDokument14 SeitenConjuntivitisOrang KalonganNoch keine Bewertungen
- PastDokument19 SeitenPastTalha Butt1Noch keine Bewertungen
- West Nile Virus Fact SheetDokument2 SeitenWest Nile Virus Fact SheetWSETNoch keine Bewertungen
- DMAS Low Acuity Non Emergent ER Diagnosis Code ListDokument17 SeitenDMAS Low Acuity Non Emergent ER Diagnosis Code ListLia TabackmanNoch keine Bewertungen
- Interstitial Lung Diseases2Dokument186 SeitenInterstitial Lung Diseases2Mohamed HefnyNoch keine Bewertungen
- SBAR ExamplesDokument2 SeitenSBAR ExamplesAriadne MangondatoNoch keine Bewertungen
- Thorax Trauma Severity Score Sebagai Prediktor Acute Respiratory Distress Syndrome Pada Trauma Tumpul ToraksDokument6 SeitenThorax Trauma Severity Score Sebagai Prediktor Acute Respiratory Distress Syndrome Pada Trauma Tumpul ToraksZeasly Tiofenly NeolakaNoch keine Bewertungen